This is basically lifted information of Ma’am Aurisita Maganis Delos Reyes’s presentation, revised into a web format/noted down using the outline method. If find it a good exercise to re-summarize this information as it was in the presentation, pointing out and organizing key points and information.
I’ll supplement information when relevant, but this is not reflective of the comprehensive information provided during her live discussions. You can find the presentation and the recorded discussions in here.
Also, forgive me for the lack of imaging used for this page. I find it difficult to seamlessly incorporate images into the page without extending page length by a lot. Google things if you’re a visual learner, especially for Assessment Tools for a Newborn, Skin Assessment, Pediatric Reflexes, and Congenital Heart Defects.
Essential Intrapartum and Newborn Care
“Essential Newborn Care” (ENC) is a part of Essential Intrapartum Newborn Care (EINC). It is a simple, cost-effective newborn care intervention that can improve both neonatal and maternal care. It is also known as Unang Yakap (First Embrace) and consists of four core steps: immediate and thorough drying, early skin-to-skin contact, properly-timed cord clamping, and non-separation of newborn from mother for early breastfeeding. Following this immediate care, six supplemental priorities take place: identification, Crede’s prophylaxis, vitamin K injection, immunization, newborn screening, and anthropometric measurement.
Immediate and Thorough Drying
Within the first 30 seconds, dry and rub the newborn, or until the newborn responds by crying. Drying acts to prevent hypothermia as the thermoregulatory capacity of the newborn is not yet stable.
- This action stimulates lung expansion and allows the nurse to assess the breathing of the newborn. Lung expansion increases pressure in the left side of the heart, which results in the closure of the fetal structures (foramen ovale and ductus arteriosus).
- Suction the airways (mouth before nose, to account for reflex breathing, for 5 to 10 seconds) only if necessary. Routine suctioning is not recommended.
- Afterwards, position the newborn prone on the mother. This can lead to an initiation of the crawling reflex, a sign of readiness for feeding.
Early Skin-to-skin Contact
From 1 minute to 30 or 60 minutes, and with the newborn on the mother, place a bonnet over the head (a major portion of heat loss comes from the head) and a blanket for the back. Benefits of skin-to-skin contact include the transfer of heat, normal skin flora, and love from the mother to the newborn.
- The period where baths are recommended is at least 6 to 8 hours after birth. Vernix caseosa, an insulator and bacteriostatic protective biofilm. It should not be washed away, as it will shed off within 24 hours. Alkaline soap is not used to wash as it rids good bacteria from the body.
Properly-Timed Cord Clamping
Late cord clamping is done 1 to 3 minutes after birth, or once placental pulsation has stopped. It is recommended as it provides additional blood—50 to 100 mL containing iron, antibodies (IgG), hormones (thyroxine, estrogen, progesterone, etc.), and enzymes for the newborn and improves oxygenation as the newborn adjusts to extrauterine life.
- Procedure: apply the cord clamp 2 cm from the base, and the forceps 5 cm from the base. The cord may be cut 1 cm from the cord clamp; 3 cm from the base. Do not milk the cord.
- Cutting of the cord results in decreased pressure in the right side of the heart, which results in the closure of the ductus venosus (1, umbilical vein to inferior vena cava) and umbilical blood vessels (2). This promotes adequate circulation and, along with lung expansion, completes the circulatory changes after birth.
- The cord should be air-dried, to prevent infection. The umbilical cord will fall off within 7 to 10 days. Betadine is not used.
Non-separation of Newborn from Mother for Early Breastfeeding
Within 60 or 90 minutes, breastfeeding prevents an estimated 19.1% of all neonatal deaths. It promotes bonding, stimulates the mother to release colostrum and breastmilk, and of the hormones prolactin (for milk production) from the APG and oxytocin (happy hormone and Let Down Reflex) from the PPG. This in turn stimulates uterine contraction, which prevents bleeding.
- It promotes uterine involution (physiologic return to pre-pregnant state)
- Breastfeeding allows the child to pass meconium earlier and more frequently (gastrocolic reflex), which promotes the excretion of bilirubin. (It’s why meconium is so yellow)
- Taurine in breastmilk promotes infant brain and intellect development.
- Breastmilk boosts the immune system, containing WBCs, macrophages, IgA, and Lactoferrin.
- Advise the mother to eat galactagogues and drink plenty of water. These are foods that promote milk production, such as oats, garlic, almonds, coconut, leafy vegetables, sago, yams, beets, carrots, green papaya, shellfish, grains, nuts, sesame seeds, and many more. Advise her to avoid peanuts, alcohol, tea/coffee, spicy foods, peppermint, high-mercury fish, and gas-inducing foods.
- Exclusive, frequent day and night breastfeeding may be used as contraception, through the Lactational Amenorrhea Method (LAM). This method is currently known to be effective for the first six months after giving birth, as it inhibits the release of FSH.
- Colostrum is the first breast milk released. It contains more antibodies and protein (lactoglobulin) than in normal breastmilk (lactalbumin). However, there are more carbohydrates in breastmilk (lactose). Both contain about the same amount of fats. Both are poor sources of iron.
- Related: R.A. 7600, the Rooming-In and Breast-feeding Act of 1992, and E.O. 51, the Milk Code.
The DO NOTs
Do not ventilate unless the baby is floppy/limp and not breathing.
Do not suction unless the mouth/nose are blocked with secretions or other material.
Do not suction meconium unless the baby is not vigorous
Do not “milk” the umbilical cord towards the newborn. This may cause circulatory overload, and contribute to jaundice.
Do not separate the newborn from the mother unless indicated (newborn does not have severe chest in-drawing, gasping, apnea; mother does not need urgent medical stabilization)
Do not place the newborn on a cold or wet surface.
Do not wipe off vernix if present.
Do not bathe the newborn earlier than 6 hours of life.
Do not do footprinting (old identification method), as it introduces a risk for contamination.
Other Priorities
- Identification: utilize double-banding (using two identifiers), ideally in the presence of the parents.
- Crede’s Prophylaxis: 1% silver nitrate (drops) or ophthalmic ointment (terramycin, gentamycin, erythromycin, penicillin) placed to protect from ophthalmia neonatorum (neonatal conjunctivitis) resulting from maternal STDs.
- Vitamin K Injection: for promotion of coagulation; prevent bleeding. The lack of normal gut flora in the newborn results in insufficient vitamin K synthesis, resulting in physiologic hypoprothrombinemia.
- Dosage: 1 mg for term/postterm newborns (0.1 mL) and 0.5 mg for preterm newborns (0.05 mL).
- Route and Site: IM, Vastus Lateralis or Rectus Femoris
- Anthropometric Measurement: the measurement of various bodily dimensions of the child to identify potential abnormalities.
- Weight is measured with an infant weighing scale.
- Length is measured from crown (posterior fontanel) to heel, following the contours of the body.
- Head circumference is measured one fingerbreadth above the eyebrows.
- Chest circumference is measured at nipple level.
- Abdominal circumference is measured at the umbilical level.
| Measurement | Normal | (SI) |
|---|---|---|
| Birth Weight | 5.5 to 7.8 lbs | 2,500 to 3,400 grams |
| Birth Length | 18 to 22 in | 48 to 54 cm |
| Head Circumference | 13 to 14 in | 33 to 35 cm |
| Chest Circumference | 12 to 13 in | 31 to 33 cm |
| Abdominal Circumference | 11 to 12 in | 29 to 31 cm |
Variance
Values change between references; in second year discussion, abdominal circumference was also 31 to 33 cm, birth length was 47 to 54 cm, and body weight was 2,500 to 4,000 grams.
- Immunization: refer to Expanded Program on Immunization.
- Newborn Screening Test: based on R.A. 9288, the Newborn Screening Act of 2004. It is done within 48 to 72 hours. The diseases screened within this act is checked to prevent mental retardation, physical abnormalities, and death.
- A Heelstick method is used to collect 4 drops of blood. The blood is analyzed within two to three weeks.
- Six diseases are screened for: Phenylketonuria, Galactosemia, G6PDD, Cretinism, Congenital Adrenal Hyperplasia (CAH), Maple Syrup Urine Disease (MSUD)
- Hearing is also screened. Sounds are played into the ears, and its response is measured. It can be done within 10 minutes and results are immediate.
Assessment Tools for a Newborn
APGAR Scoring
Wong's Nursing Care of Infants and Children, pp. 199-200
Created by Dr. Virginia Apgar, this is a screening test done one minute and five minutes after birth. The first test is to determine the newborn’s ability to cope with the birthing process, and the second test is done to determine the newborn’s ability to adjust to extrauterine life. This test determines the degree of acidosis and aids in determining the need for CPR.
| Criteria | Score of 2 | Score of 1 | Score of 0 |
|---|---|---|---|
| Appearance | Pink | Acrocyanosis (extremities are blue) | Central cyanosis or pallor |
| Pulse | >100 BPM | <100 BPM | No pulse |
| Grimace | Cries, sneezes, pulls away | Grimaces or weak cry | No response |
| Activity | Active movement; well flexed | Some flexion of extremities | Flaccid/limp; no movement |
| Respiration | Good, strong cry | Weak cry; slow/irregular | No breathing |
The score is tallied, and interpreted as:
- 0 to 3: poor, serious, severely depressed. CPR may be required.
- 4 to 6: fair, guarded, moderately depressed. Suctioning may be required. Monitoring is required.
- 7 to 10: good, healthy.
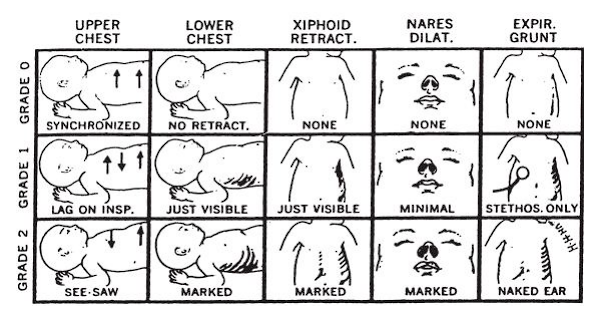
Silverman-Anderson Index
Also known as Silverman-Anderson Respiratory Severity Score (RSS). It evaluates five parameters of work of breathing and assigns an overall score with a patient breathing comfortably a 0 and a patient in severe respiratory distress a 10.
| Scoring | Upper Chest | Lower Chest | Xiphoid Retract | Nares Dilate | Expiratory Grunt |
|---|---|---|---|---|---|
| 0 | Synchronized | No retraction | None | None | None |
| 1 | Lag on respirations | Just visible | Just visible | Minimal | Audible on Stethoscope Only |
| 2 | See-saw Respirations | Marked | Marked | Marked | Audible by Naked ear |
| The score is tallied, and interpreted as: |
- 0 to 3: good, healthy, no respiratory distress.
- 4 to 6: fair, guarded, mild respiratory distress.
- 7 to 10: poor, serious, severely respiratory distress.
A visualization:
Ballard Scoring
Wong's Nursing Care of Infants and Children, pp. 202-203
Evaluates gestational maturity based on neuromuscular maturity and physical maturity.
Neuromuscular maturity is determined by observing:
- Posture: with infant quiet and in a supine position, observe degree of flexion in arms and legs. Muscle tone and degree of flexion increases with maturity. Score: Full flexion of arms and legs = 4.
- Square Window (Wrist): with thumb supporting back of arm below wrist, apply gently pressure with index and third fingers on dorsum of hand without rotating infant’s wrist. Measure angle between base of thumb and forearm. Score: Full flexion (hand lies flat on ventral surface of forearm) = 4
- Arm Recoil: with infant supine, fully flex both forearms on upper arms, hold for 5s; pull down on hands to fully extend and rapidly release arms. Observe rapidity and intensity of recoil to a state of flexion. Score: A brisk return to full flexion = 4.
- Popliteal Angle: with infant supine and pelvis flat on a firm surface, flex lower leg on thigh and then flex thigh on abdomen. While holding knee with thumb and index finger, extend lower leg with index finger of other hand. Measure degree of angle behind knee (popliteal angle). Score: an angle of less than 90° = 5
- Scarf Sign: with infant supine, support head in midline with one hand; use other hand to pull infant’s arm across the shoulder so that infant’s hand touches shoulder. Determine location of elbow in relation to midline. Score: elbow does not reach midline = 4.
- Heel-to-Ear: with infant supine and pelvis flat on a firm surface, pull foot as far as possible up toward ear on same side. Measure distance of foot from ear and degree of knee flexion (same as popliteal angle). Score: knees flexed with a popliteal angle of less than 10° = 4.
Physical maturity is determined characteristically based on neonatal skin, presence of lanugo, the plantar surface, breasts, eye and ears, and genitals. Expected appearance for pre-term, term, and post-term are:
| Preterm | Term | Postterm | |
|---|---|---|---|
| Skin | Gelatinous, transparent; visible blood vessels | Smooth, pink, superficial cracking, less visible veins | Parchment-like, deep cracking, no visible blood vessels |
| Ear Cartilage | Absent/Pliable | Formed and firm with instant recoil | Thick cartilage; stiff |
| Breast Nodule | 1-2 mm | 3-5 mm | 6-10 mm |
| Genitals (Male) | Undescended; less swollen testes. Few rugae. | More swollen; more rugae | Fully descended; pendulous (swings). Markedly swollen. Extensive rugae. |
| Genitals (Female) | Clitoris and minora prominent | Majora partially covers | Majora completely covers minora and clitoris. |
| Sole Creases | Only anterior and transverse surfaces have creases | 2/3 of the sole has creases | The entire sole has creases. |
| Lanugo | Abundant | Less Lanugo | No Lanugo. |
The actual form with visualizations can be found here. The form is based on the New Ballard Score by J.L. Ballard et al. in 1991.
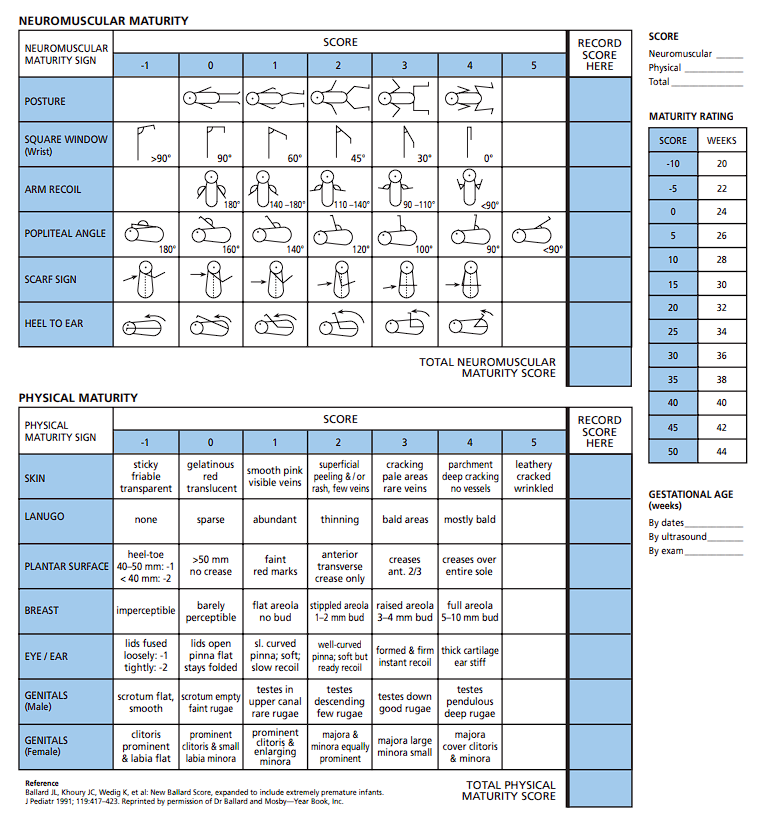 Note the interpretation for Maturity Rating: a score of less than 35 is preterm (36 weeks and below), 35 to 45 is term, and above 45 is post-term.
Note the interpretation for Maturity Rating: a score of less than 35 is preterm (36 weeks and below), 35 to 45 is term, and above 45 is post-term.
Vital Signs
- Respiratory Rate: normally 80 breaths/min soon after birth, stabilizing to 30-60 breaths/min. The breathing of a newborn is normally rapid, irregular, with normal physiologic apnea of <15 seconds in a minute. They are shallow but quiet, and abdominal/diaphragmatic.
- Pulse Rate: normally 180 BPM, stabilizing to 120-160 BPM. It is also rapid and irregular, increasing with crying and decreasing during sleep. The sites for pulse rate observation in a newborn may be at the apical pulse, brachial pulse, femoral pulse, (if weak, this suggests CoA), and pedal pulse.
- Temperature: the thermoregulating center of a newborn is immature. Reasons for difficulty in maintaining temperature include an underdeveloped shivering mechanism, inadequate adipose tissues, and large surface area, making newborns more prone to heat loss. The normal temperature of a newborn is 36.4°C to 37.2°C (Prof. says 36.5°C to 37.5°C). It takes 6 to 8 hours after birth for temperature to stabilize.
- Complications of hypothermia:
- Hypoglycemia: normally 30 to 65 MG%
- Metabolic acidosis
- Respiratory Distress
- Complications of hypothermia:
- Blood Pressure: normally 80/46 mm Hg at birth, increasing to 100/50 in 10 days. When measured, it is normally higher in the lower extremities than in the upper extremities. Otherwise, this also suggests a congenital heart defect (CoA). Measurement may be via doppler or flush methods.
- Blood pressure monitoring is optional in a newborn, but is required at 3 years old.
Physical Examination
The assessment for a newborn does not follow the usual cephalocaudal direction. It is used starting in preschoolers (4 to 6 years old). For younger children, the chest is the first target, before proceeding with the head. This discussion utilizes a assessment-based approach, categorizing normal and abnormal findings based on the body system being assessed. Particularly lengthy discussions on abnormalities will be in their own section. Some systems had minimal discussions, so forgive me for insufficient material.
Chest Assessment
The chest should not show retractions, and have clear symmetrical breath sounds throughout all lung fields.
Abnormalities
- Retractions: visual inspection for retractions that may indicate respiratory distress.
- Breath Sounds: auscultate the lungs for breath sounds.
- If absent, the lungs are not expanding; collapsed lungs or atelectasis.
- Wheezes, especially upon expiration, may indicate a lower respiratory tract obstruction.
- Stridor, high-pitched adventitious sounds upon inspiration indicates an upper respiratory tract obstruction.
- Rales or crackles are rattling, bubbling, or clicking sounds. This is commonly found in fluid or secretory obstruction in the lungs.
- Witch Milk: colorless or transparent fluid expressed by the neonatal mammary glands caused by maternal hormones.
Head Assessment
Two important landmarks of the hear are the fontanels. There are six in total: the anterior fontanel, the posterior fontanel, two sphenoid (anterolateral) fontanel, and two mastoid (posterolateral) fontanel.
- The anterior fontanel is diamond-shaped and 3-4 cm long and 2-3 cm wide. If the fontanel is larger than 5 cm, it may indicate hydrocephaly or cretinism. It closes within 12 to 18 months, as early as 9 months. Earlier closure is termed “Craniostenosis”.
- The posterior fontanel is triangle-shaped and measures 2 cm long and 1 cm wide. It closes within 2 to 3 months. It is pulsatile and flat. Bulging may indicate increased ICP, but bulging while crying is normal. If the fontanel is depressed/sunken, it may indicate dehydration.
Abnormalities
- Craniosynostosis/Craniostenosis: premature closure of the fontanels and sutures. It can limit brain growth and available volume in the skull. This can increase ICP, result in mental retardation and brain herniation (through the foramen magnum), and death.
- Caput Succedaneum: swelling of the scalp caused by a prolonged second stage of labor. This swelling affects both sides, crossing the suture line. There is no special treatment required, as it normally resolves within two to three days.
- Cephalhematoma: collection or accumulation of blood caused by a rupture of periosteal capillaries. It does not cross the suture line, only affecting one hemisphere. It disappears in three to four weeks. The bleeding can contribute to jaundice.
- Craniotabes: localized softening of the cranial bones. It is commonly seen in early lightening and firstborn babies. It disappears in six weeks.
- Molding: overlapping cranial bones after birth as the bones squeeze together to pass through the birth canal. This is common among preterm babies.
Face Assessment
Observe the newborn’s face for symmetry. It should be primarily symmetrical, with only mild asymmetries. If the face is markedly asymmetrical, it can indicate facial nerve (CN VII) paralysis i.e. Bell’s Palsy.
- Eyes: pupils should be normally equal, round, reactive to light, and shows accommodation (PERRLA). The lacrimal duct in newborns is immature, so no tears form.
- Tests for blindness should done within the first ten days of life: Doll’s Eye Test (move head laterally; eyes should move in the opposite direction, indicating intact brain stem function) and Glabellar Tap Test (tap just above the nose; the eyes should blink as a protective reflex, also discussed in Pediatric Reflexes).
- Nose: the primary sign to look for from the nose is nasal flaring. Enlarged nares can indicate respiratory distress. This may be caused by obstruction by secretions, bone, or membranes (choanal atresia); or a lack of surfactant production.
Abnormalities
- Bell’s Palsy: paralysis of the facial nerve (CN VII). Management aims to prevent the premature disappearance of the sucking reflex. For this, the baby is fed with dropped and syringe, and encouraged to breastfeed. Aspiration precautions are applied.
- Coloboma: a keyhole appearance of the eyes from a hole formed in one of the structures of the eyes.
- Exotropia Strabismus: wall-eyed defect (◐‿◑) of the eyes, and Esotropia Strabismus: cross-eyed defect (◑‿◐) of the eyes. Non-physiologic strabismus is managed with occlusion therapy, surgery (SQUINT), corrective glasses, and laser therapy.
- Respiratory Distress Syndrome, A.K.A. Hyaline Membrane Disease. Its cause is unknown, but its predisposing factors include prematurity, LBW/SGA/LGA, and CS delivery.
- Craniofacial Defects: defects in the formation of the facial structures, such as a Cleft Lip/Palate deformity. Also found in Down Syndrome.
Respiratory Distress Syndrome
Also known as hyaline membrane disease, it is a disorder in the respiratory system of a newborn whose cause is unknown. Its predisposing factors include premature babies; LBW, SGA, and LGA babies; and CS delivery babies.
Management
- Continuous Positive Airway Pressure (CPAP): maintained positive airway pressure that keeps the alveoli open, preventing atelectasis.
- Oxygen Therapy: 40% FiO₂ (not higher, to prevent blindness/retrolental fibroplasia and emphysema/bronchopulmonary dysplasia).
- Incubation to provide a warm environment, allowing the newborn to conserve energy and avoid infection (via isolation). It is set at 34.4°C with a humidity of 55% to 65%. Minimal handling should be done, while utilizing touch therapy.
- Medication: steroids to promote surfactant maturation (Dexamethasone, Betamethasone), exogenous surfactant administration (Beractant) intratracheally, sodium bicarbonate for correction of acidosis, and gamma immunoglobulin.
- Monitoring: watch for anemia (BT, 50 mL PRBC), hyperbilirubinemia (Phototherapy, exchange transfusion), and malnutrition from excessive oxygen utilization, resulting in poor growth and development (TPN, Gavage, Breastfeeding)
Ear Assessment
The position of the ears is determined in relation to the line of the inner and outer canthus of the eye. Ears that are set lower than normal is abnormal, and can be seen in chromosomal defects such as Down syndrome, Patau syndrome, Edward disease; kidney defects; and craniofacial defects.
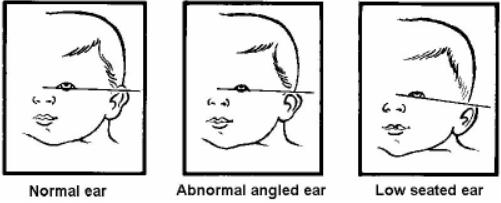
Abnormalities
- Down Syndrome: one of the characteristic appearances of Trisomy 21 is a low-set ear placement.
Down Syndrome
Trisomy 21, whose cause is unknown, but with the predisposing factors of advanced maternal age. Trisomy 21 indicates the presence of three 21st chromosomes, totaling 47 chromosomes rather than the expected 46. The expected lifespan of those with down syndrome is variable.
Assessment Findings
Down syndrome contains highly characteristic mental retardation and physical abnormalities, such as:
- Microcephaly
- Low-set ears
- Saddle nose
- Small mouth with macroglossia
- Short neck
- Short and stubby digits with single transverse line (simian crease)
- Hypotonic musculature
- Protuberant abdomen
- Small penis with cryptorchidism
Down syndrome commonly involves defects that can result in disability and dysfunction:
- Cardiac Defects: refer to Congenital Heart Defects
- Gastrointestinal Tract Defects: esophageal atresia
- Gastrourinary Tract Defects
Diagnostic Tests
- Alpha fetoprotein (AFP): a protein created by a growing liver, normally high in an unborn child. Testing of AFP presence in maternal serum can reveal low levels, indicating a potential genetic abnormality.
- Chorionic Villi Sampling: checks cells from the placenta (which are identical to cells from the fetus) to see if they have a chromosomal abnormality.
- Karyotyping: genetic testing to reveal the presence of extra or missing chromosomes.
Mouth Assessment
Observe the oral cavity for abnormal mucous membranes, secretions, odor, and appearance/structure. Craniofacial defects can also implicate the mouth, such as in the case of a Cleft Lip and Cleft Palate.
Abnormalities
- Epstein Pearls: white glistening epithelial cysts at the palate and gums, causing by extra loads of calcium.
- Teeth can be found if vitamin intake was excessive. They are extracted to prevent aspiration if they fall out, especially if neonatal reflexes have not yet developed.
- Vomiting can be projectile or non-projectile:
- Projectile: commonly caused by obstructive defects such as Pyloric Stenosis, Intussusception, and Aganglionic Megacolon.
- Non-projectile: commonly caused by non-obstructive defects such as infections, or chalasia (weakness of the lower esophageal sphincter)/GERD.
- Cleft Lip/Palate: a malformation of the lip/palate in a newborn. It is commonly genetic or due to maternal folic acid (Vitamin B₉) deficiency.
- Esophageal Atresia can be suspected by excessive drooling.
- Oral Moniliasis/Candidiasis: caused by the bacteria Candida albicans, a fungus potentially acquired by the baby during passage through the birth canal. Management is mainly pharmacologic with antifungals (Nystatin) applied to the oral cavity with a gloved finger.
Cleft Lip and Cleft Palate
A malformation of the lip and/or palate. It is known to be genetic, or caused by maternal folic acid (B₉) deficiency. If uncorrected, it can result in feeding difficulties, speech defects, dental defects, altered normal body image, or even respiratory distress. The compromised tissues can also result in upper respiratory and ear infections (through the eustachian tube).
Surgical Management
A cheiloplasty or palatoplasty is used to reconstruct the closure of the unformed tissues. Nursing responsibilities during the preoperative phase include:
- Proper positioning during and after feeding: upright.
- Burp or bubble the newborn more often.
- Feeding utilizes cross-cut large holed nipple or Breck feeder technique.
- Monitor for complications: otitis media, etc.
- Orthodontic exercise and surgery for dental defects
- Speech therapy
During the postoperative phase, nursing care includes:
- Proper Positioning: prone if a cleft palate repair is done, and side-lying or supine if a cleft lip repair is done. An elbow restraint is used, released every two hours.
- Feeding with a rubber-tipped medicine dropper for cleft lip repari, and paper cups and soup spoon for cleft palate repair.
- Wound cleaning with hydrogen peroxide.
- Medications, including prophylactic antibiotics and analgesia.
- Avoiding incision disruption includes avoiding sucking (esp. for Logan’s Bar/Bow), suctioning, blowing, and any foreign object in the mouth.
Esophageal Atresia
It is the failure of the esophagus to form a continuous passage between the mouth and the stomach. It is a congenital defect often associated with other defects, warranting the assessment of other defects: (mn. VACTERL, VERT(i)CAL) vertebral, anorectal, cardiovascular, tracheal, esophageal, rectal, and limb defects. Its cause is unknown, but is also common in Down Syndrome.
- Diagnosis is done via x-ray.
Assessment Data
- Excessive drooling of saliva
- Choking after initial feeding
- Resistance upon NGT insertion
- Respiratory distress from secondary aspiration
- Abdominal distention: air trapping from tracheal fistulae connecting to the distal esophagus
- Cyanosis/tachypnea
- History of maternal polyhydramnios as the fetus does not swallow extra amniotic fluid. Approximately one-third of fetuses with esophageal atresia are found to have maternal polyhydramnios.
Medical Management
Surgery may be necessary depending on the type of defect. The creation of a gastrostomy or cervical esophagostomy can establish a patent esophagus. Fistulae are divided and the ends of the esophagus are anastomosed, before the gastrostomy is closed.
Nursing Management
Proper positioning (elevate head at 20° to 30°) is used to prevent aspiration. Regular suctioning is done.
- Administer oxygen if cyanosis occurs.
- Administer TPN as ordered (IV Hyperalimentation) as the primary source of nutrition.
Pyloric Stenosis
The narrowing of the pylorus/pyloric sphincter, which restricts gastric emptying and results in projectile vomiting in a newborn. It is the pyloric muscle that enlarges and thickens, decreasing the lumen of the pylorus. The stomach becomes a palpable olive-shaped mass and compensating peristalsis becomes visible. The child becomes irritable and restless.
- Surgery may be required to correct the stenosis. The Fredet Ramsted Procedure, a pyloromyotomy to separate hypertrophied pyloric muscle without any mucosal incision, releases the restriction of the pylorus. This is done with a laparoscope.
Nursing Management
- Feedings use thickened formula (rice cereal and milk) given through gavage.
- Prevent and correct dehydration from vomiting, with the potential use of IVF. Measure I&O.
- Monitor for complications such as metabolic alkalosis, acidosis, and dehydration.
Neck Assessment
The neck is often short in newborns. Notably, it is the site where the thyroid gland can be found. The nurse palpates for the thyroid gland, though it is normally not palpable in a newborn. A thyroid scan exposes T₃ (triiodothyronine) and T₄ (thyroxine) levels which, if low, diagnoses cretinism.
Abnormalities
- Cretinism: insufficient thyroid hormone production, potentially from iodine deficiency. This is one of the disorders tested in newborn screening as it can result in mental retardation. Treatment is hormone replacement therapy with Synthroid.
- Congenital Torticollis: “wry neck”; abnormal contractions of the sternocleidomastoid (SCM) muscle, resulting in twisting of the neck. It may be treated with exercise and the application of warm packs or compress, but in severe cases, a tenotomy may be done to release the contracted muscle.
Abdominal Assessment
The abdomen is normally dome-shaped and cylindrical. The stomach, at birth, is able to store ~90 mL, with rapid peristalsis (can commonly reverse as well) and short emptying time. Absorption is faster in the small intestines as they contain more secretory glands and a larger surface area. There are various palpable organs:
- Liver: 2 to 3 cm below the right costal margin.
- Kidneys: 1 to 2 cm above the umbilicus.
- Spleen: in the left upper quadrant.
Abnormalities
- Diaphragmatic Hernia: a herniation is the protrusion of an organ outside of its normal cavity. In the case of a diaphragmatic hernia, parts of the intestines can be pushed into the thorax, which can lead to the collapse of the lungs. It may be left-sided (Bochdalek Hernia) or right-sided (Morgagni Hernia).
- Omphalocele: the protrusion of abdominal organs through the umbilicus. The herniated organs are often contained by a sac, but is prone to infection. Until corrected, the nurse covers the defect with sterile saline dressing, preferably changed every two hours.
- Gastroschisis: the protrusion of abdominal organs through the abdomen via a defect or hole in the abdominal wall. The herniated organs are also very prone to infection (administer prophylactic antibiotics), and is reduced using a silastic silo (covering for the protruded organs, which reduces expulsion and maintains sterility until surgical repair is done.
- An overhead warming unit is used as the exposed organs increase heat loss.
- Intussusception is the telescoping self-insertion (invagination) of a section of the intestine. This is an obstructive disorder which results in pain (earliest sign) and projectile vomiting in newborns (bilous, fecaloid). These can form within three weeks of life.
- Palpation reveals a sausage-shaped mass in the abdomen, and the passage of currant jelly-like (bloody and mucoid) stool.
- Diagnosis reveals a coiled spring or staircase sign via a lower gastrointestinal series or barium enema.
- Treatment: barium enema, bowel milking, or if indicated, bowel resection with end-to-end anastomosis.
- Hirschsprung’s Disease/Aganglionic Megacolon: absent nerve cells (ganglions) in a section of the bowel which results in the loss of peristaltic movement.
Diaphragmatic Hernia
Parts of the intestines are pushed into the thorax, crowding the lungs, which can lead to lung collapse. It may be left-sided (Bochdalek Hernia) or right-sided (Morgagni Hernia).
Assessment Findings
- Dyspnea, tachypnea, and tachycardia from compromised lung volume.
- Cyanosis
- Asymmetrical chest development
- Concave abdomen from reduced volume, as some parts have herniated upwards.
- Asymptomatic cases can be found in those with a Morgagni Hernia, as the right lung has a higher capacity, as the left lung is already compensating the presence of the heart.
Medical Treatment
Diaphragmatic herniation is an indication for neonatal intensive care. The use of a mechanical ventilator may be required due to the compromised lung capacities, or even potentially an extracorporeal membrane oxygenator (ECMO). Surgery is used to correct the herniation.
Aganglionic Megacolon
Also known as Hirschsprung’s Disease, this is the absence of nerve cells (ganglions) in a section of the bowel results in the loss of peristaltic movement. Intestinal materials accumulate in the aganglionic section, and results in a megacolon/obstruction.
Assessment Findings
- Non-passage of meconium; passing of ribbon-like or pellet stool. Chronic constipation can be observed.
- Projectile vomiting
- Abdominal distention and shortness of breath
- Anorexia
Surgical Management
A colostomy is instated temporarily before a Swenson and Soave Procedure, followed by colostomy closure. Preoperatively, the nurse:
- Provides a daily enema (olive oil/diluted antibiotics for retention edema; NSS for non-retention edema).
- Feeds the child small, frequent low-residue feedings
- Measures abdominal circumference daily
- Elevates the head to ease breathing.
- Administer medications as ordered, e.g. stool softeners.
- Provides oral hygiene and psychosocial support
Anogenital Assessment
Assessment of the anus, rectum, perineum, and some parts of the genital system.
- The newborn is expected to pass meconium within 24 hours. Failure to do so can indicate obstruction (Imperforate Anus, Aganglionic Megacolon, Cystic Fibrosis)
- Stool varies with types: meconium (green-black, sticky, odorless, passed four times a day), transitional (yellow-green, slimy, six or more times a day), breast-fed baby stool (golden-yellow, mushy, soft, sweet odor, passed after feeding), and bottle-fed baby stool (pale-yellow, hard, formed, foul odor, passed once a day.)
Abnormalities
- Imperforate Anus: the non-formation of the anal passage, often with an associated fistula to the genitourinary system. It is suspected if the anal opening is observed to be absent or misplaced, if no stool has passed within 24 to 48 hours of life, or if stool has been passed elsewhere (vagina, base of the penis, scrotum, or urethra). Abdominal distention also results from the lack of stool passage. Surgery is used to correct the defect:
- Colostomy (Stage I) followed by a pull-through procedure (Stage II), followed by the closure of the colostomy (Stage III).
Urogenital Assessment
Assessment of the reproductive system, external genitalia, and internal structures (kidneys).
Abnormalities
- The newborn is expected to void six to eight times within the first 24 hours, and twelve to twenty times daily after. Failure to do so may suggest renal agenesis (non-formation of the kidneys), dehydration or an absence of the urinary meatus.
- Abnormalities of the meatus can result in altered direction or outflow of urine:
- Epispadias: the meatus opens atop the penis.
- Hypospadias: the meatus opens below the penis.
- Non-descent of the testes is checked with palpation of the scrotum. If the testicles are found to be undescended, a disorder known as cryptorchidism is determined. A complication of this condition is inguinal hernia, testicular cancer, and sterility.
- HCG and Testosterone as HRT can correct cryptorchidism. If necessary, surgical intervention (orchiopexy/orchidopexy) can be done to move the undescended testes into the scrotum.
- Transillumination of the scrotum can reveal clear fluid within the scrotum. This is intraabdominal fluid leaking into the scrotum, which is termed as a hydrocele. If a loop of intestines is also found within the scrotum, it is termed as a scrotal hernia.
- A hydrocele may be typed as non-communicating (closed off) or communicating (open; may result in herniation). The latter requires elective repair to prevent complication.
- Phimosis is present in most male babies. The foreskin is never retracted as it may cause laceration. This usually disappears within 6 months to 1 year, otherwise it will be treated with circumcision.
- Pseudomenstruation (false menstruation) may be observed in female babies, caused by the withdrawal of maternal hormones.
- Uric Crystals can be caused by urates, and appear as pink or brick-red crystals.
Extremity Assessment
The extremities are assessed for symmetry in movement, presence, and malformation. The movements of the extremities should be symmetrical, with asymmetry suggesting weakness or paralysis (commonly Erb’s palsy or Brachial Plexus Paralysis)
- The legs of a newborn are normally bow-like; bow-legged (varus) until toddlerhood.
- The feet of a newborn are flat due to fat deposits and usually point outward, but will be corrected (straight upward) by the time the child is ready to walk. The direction the foot points in and its general formation can be abnormal (Equinous, Varus, Valgus, Calcaneous)
Abnormalities
- Erb’s Palsy/Brachial Plexus Paralysis: damage to the brachial plexus nerve, which can limit the use of the arm. Damage commonly occurs during delivery. In the affected arm, the moro reflex is absent, the tonic neck reflex is incomplete, and there is decreased sensory and motor function. Infant reflexes are discussed here.
- The affected arm is abducted and rotated externally, then immobilized with a figure of eight or airplane splint.
- Amelia: absence of an entire limb
- Phocomelia: absence of arms or legs
- Hemimelia: absence of hands or feet
- Hip Dysplasia or Hip Dislocation tested with the Ortolani test, a test for hip dislocation (reduction). The examiner holds the hip and applies anterior pressure to flex the thigh on the hip, then rotates the thighs outward. If hip dysplasia is present, the head of the femur moves back into place. The Ortolani sign is a distinct click or clunk heard when the head of the femur slips forward in the acetabulum if hip dysplasia is present. The femur becomes displaced again once pressure is released.
- Casts and traction can be used to treat hip dysplasia/dislocation: hip spica cast, Bryant’s Traction.
- Equinous: downward-pointing toes (plantar flexion).
- Varus: inward-pointing toes (inversion).
- Valgus: outward-pointing toes (eversion).
- Calcaneus: upward-pointing toes (dorsiflexion).
- Equinovarus, a combination of equinous and varus malformations, is also known as Clubfoot, and is the most common defect. It is characterized by plantar flexion (downward-pointing toes) and inversion (inward-pointing toes). It may be managed with:
- Exercise
- Casting
- Arthrodesis
- Dennis Browne Application
Back Assessment
The back should be flat and straight. The lumbar curve only forms at six months of age.
Spina Bifida
Tufts of hair, dimples, or masses can indicate spina bifida. It is a deformity resulting from the incomplete closure of the vertebrae, allowing the protrusion and leakage of spinal components. This can also contribute to hydrocephaly.
- Spina Bifida Occulta: a hidden deformity, which can still be manifested by a tuft of hair, a dimple, or a small mass.
- Spina Bifida Cystica: a protrusion of the spinal contents through the open vertebral structure. This can be further classified according to the contents of the protrusion:
- Meningocele: protrusion of the meninges and cerebrospinal fluid.
- Myelomeningocele: protrusion of meninges, cerebrospinal fluid, nerve roots, and part of the spinal cord.
- Rachischisis: protrusion of the meninges and spinal cord.
- Hydrocephalus: an abnormal enlargement of the head from the retention of fluid within the cerebral ventricles.
Surgical Management
The sac is excised if possible. Surplus CSF is drained via a shunt to prevent ICP elevation. The shunt may be ventriculoperitoneal or ventriculoatrial. It is the duty of the nurse to observe for signs of shunt malfunction.
Nursing Management
The protruding sac should be protected from rupture. This can be done through positioning (prone with hips abducted and head slightly elevated), the application of a sterile donut ring around the sac, and covering the sac with sterile saline dressing changed every two hours.
Increased ICP related to hydrocephalus include characteristic physical manifestations:
- Macewen’s Sign a cracked pot sound
- Bossing Sign: a protruberant forehead
- Sunset: the iris is positioned lower than the sclera; the white of the eye is visible above the iris.
- Bulging and Tense Fontanels
- High Pitched and Shrill Crying
- Altered level of consciousness
- Changes in VS
Skin Assessment
The skin is assessed for its color and marks. The skin at birth is normally pink, potentially due to high RBC. Normal CBC values for an infant are:
- RBC: 4.4 to 7.5 million/mm³
- Hgb: 14.5 to 22.5 g/dL
- Hct: 45% to 65%
- WBC: 5,000 to 35,000/mm³
Abnormalities
- Cyanosis: blue/purple discoloration of the skin resulting from hypoxia.
- Pallor: paleness of the skin resulting from anemia, potentially due to ABO or Rh incompatibilities, hemolytic disorders, and bleeding. The decreased synthesis of Vitamin K can contribute to hemophilia, a deficiency or absence of clotting factors conducive to excessive bleeding. It may also be due to a deficiency in platelets.
- Jaundice: a yellow discoloration of the skin resulting from heightened levels of bilirubin. There are two types, physiologic (normal) and pathologic (abnormal):
| Parameter | Physiologic Jaundice | Pathologic Jaundice |
|---|---|---|
| Onset | 2nd day | 1st day |
| Duration | to 7 days (or to 14 for preterm babies) | More than 7 days (or more than 14 if preterm) |
| Bilirubin | 5 mg/day 12 mg/day on 3rd day | >5 mg/day 12 mg/day |
| Treatment | Sunlight and phototherapy | Phototherapy and exchange transfusion |
- Nevus Vasculosis (Strawberry marks) are elevated areas formed by immature capillaries and endothelial tissues.
- Nevus Flammeus (Portwine Stains): a macular purple or dark-red lesion or patches. It can be seen on the face, buttocks, thigh, and genitals.
- Tangiectasis Nevus: a flat, red area of capillary dilatation commonly seen at the glabella, upper eyelid, and upper lip.
- Mongolian Spot: a slate blue or gray patch caused by the accumulation of melanocytes commonly seen at the buttocks and back. This normally disappears by preschool age.
- Lanugo: fine downy hair seen at the back, upper arm, and shoulder. These are common in preterms as they often disappear by the eighth month of gestation. This disappears within two weeks.
- Vernix Caseosa: a white, cheesy substance seen all over the body that aids in delivery, thermoregulation, and acts as a bacteriostatic agent. This normally disappears within 24 hours.
- Erythema Toxicum: pink papules with superimposed vesicles seen on the face. This disappears in two weeks and is commonly the first rash of the newborn.
- Milia: small white spots commonly seen at the tip of the nose caused by clogged sebaceous glands. These are the whiteheads of the newborn.
- Desquamation: dry peeling-off of the skin
Pediatric Reflexes
Reflexes are involuntary movements or actions. Some appear spontaneously, and some can be elicited by specific stimuli or positions. The assessment of reflexes helps identify normal brain function and nerve activity.
- Moro Reflex: also known as the embrace or startle reflex. It may be elicited by jarring the crip, dropping an object, or allowing the head of the baby to drop by a 30° angle.
- The baby extends the arms with the hands open, with the middle finger and the thumb forming a “C” shape.
- The absence of the moro reflex indicates a neurological problem.
- Tonic Neck Reflex: also known as the fencing reflex. It can be elicited by turning the head to one side.
- The baby extends the arm in the direction the head is turned, while flexing the other arm (as if fencing! 🤺)
- Crawling Reflex: elicited by placing the baby prone.
- The baby bends the knees and attempts to move forward.
- Stepping/Dancing Reflex: elicited by holding the baby upright. It is believed to prepare the baby developmentally for walking.
- The baby begins to take steps and “dance” when set on a solid surface.
- Babinski Reflex: elicited by stroking the underside of the foot of the baby from the hell towards the big toe in an inverted “J” curve fashion.
- The baby’s toes fan out, with the big toe curved upward.
- Plantar Reflex: elicited by an object placed beneath the toes.
- The baby’s toes curls around the object placed beneath the toes, similar to the grasping reflex.
- Grasping/Palmar Reflex: elicited by touching the anterior surface of the hand.
- The baby grasps the object placed on the hand.
- Landau Reflex: elicited by holding the infant in a prone position.
- The baby raises their head and extend the neck and trunk, with the entire body flexing when the neck is passively flexed.
Feeding Reflexes
- Rooting Reflex: elicited by stroking the cheek or the corner of the mouth with an object. The baby responds by moving its head toward the object, locating it.
- Extrusion/Protrusion/Spit Out Reflex: elicited by placing an object on the anterior surface of the tongue. The baby responds by pushing the object away from the mouth, protecting the baby from aspiration.
- Sucking/Suckling Reflex: elicited by placing an object between the lips. The baby responds by opening the mouth and grabbing the object.
- Swallowing Reflex: the sequential activation of the tongue, pharyngeal and laryngeal muscles to propel milk from the oral cavity into the esophagus while avoiding aspiration.
Protective Reflexes
- Glabellar/Blinking Reflex: elicited by tapping on the forehead just above the nose. The baby blinks or closes their eyes to protect them.
- Gag Reflex: a reflex action to prevent choking, potentially triggered by fingers, food, a spoon, or toys.
- Sneezing Reflex: a sneeze just like in adults (this reflex that does not diminish) when the nasal passages are irritated.
- Coughing Reflex
| Reflex | Duration |
|---|---|
| Stepping/Dancing | 2 months |
| Rooting | 3 to 4 months |
| Moro | 4 to 5 months |
| Extrusion/Protrusion/Spit Out | 4 to 5 months |
| Grasping/Palmar | 5 to 6 months |
| Tonic Neck/Fencing | 5 to 7 months |
| Sucking/Suckling | 6 months |
| Plantar | 9 to 10 months |
| Crawling | 10 months |
| Babinski | 12 to 18 months |
| Landau | 12 to 24 months* |
| Glabellar/Blinking | Disappears in the mature brain* |
| Swallowing, Sneeze, Cough, Gag | Stays until adulthood |
Items suffixed with * are externally sourced.
Congenital Heart Defects
Congenital heart defects (CHDs) are malformations of the heart, e.g. from formation or from non-closure of fetal vascular structures such as the ductus arteriosus. They may be categorized into two types based on the presence of cyanosis, a manifestation of markedly impaired oxygenation.
Children with CHDs tire quickly and experience dyspnea. With exertion, cyanosis can become severe and syncope can occur (hypercyanotic spells). Decreased cardiac output and oxygenation also results in:
- Edema
- Diaphoresis
- Oliguria
- Growth Retardation
Care for children with CHDs is primarily focused on the principle of improving cardiac function, cardiac output, and decreasing cardiac workload and edema. Overall, these all improve tissue perfusion.
Acyanotic CHDs
These are CHDs that do not produce cyanosis. This is because the defects under this type of CHD create left-to-right shunting, which transfer oxygenated blood back into pulmonary circulation. Tissue perfusion is not significantly compromised. Findings include decreased CO₂, congestive heart failure, and left ventricular hypertrophy.
- Atrial Septal Defects (ASD): a hole is present in the arterial septum, the wall between the left and right atria.
- Ventricular Septal Defects (VSD): a hole is present in the ventricular septum, the wall between the left and right ventricles.
- Patent Ductus Arteriosus (PDA): a hole that connects the aorta and the pulmonary artery is present.
- Coarctation of the Aorta: a narrowing of the aorta constricts blood flow to the lower body, increasing upper body and extremity hypertension. It does not greatly affect oxygenation, but can result in cardiac dysfunction later in life.
Cyanotic CHDs
These are CHDs that produce cyanosis. This is because the defects under this type of CHD create right-to-left shunting, which allow deoxygenated blood to enter systemic circulation, bypassing oxygenation in the pulmonic circulation. Tissue perfusion can be significantly compromised. Findings include cyanosis, decreased cerebral and peripheral perfusion, polycythemia, and multiorgan malfunction.
- Tetralogy of Fallot (TOF): a combination of a VSD, an overriding aorta (both ventricles can pump blood into the aorta), pulmonary stenosis (restricting cardiac output into pulmonic circulation), and right ventricular hypertrophy.
- Transposition of the Great Arteries (TGA): swapping of the aorta (heads to lungs) and pulmonary artery (heads to body) connections, resulting in two closed circulating loops of pulmonic circulation and systemic circulation. The only saving grace for circulation are more defects, e.g., a patent foramen ovale, or VSD that allow oxygenated blood to cross into systemic circulation.
- Truncus Arteriosus: the presence of a common arterial trunk, where the aorta and main pulmonary artery merge into one large artery distributing mixed blood.
- Tricuspid Atresia: the non-formation of the tricuspid valve, resulting in non-communication between the right atrium and right ventricle. The right ventricle, not having adequate volume, remains small, and is only able to receive blood from the presence of an ASD and VSD, which allow blood to travel from the right atrium, to the left atrium, to the left ventricle, then to the right ventricle, before entering pulmonic circulation.
Diagnostic Examination
- Imaging is done via CXR, and a 2D ECHO.
- ABGs analyze the child’s oxygenation and level of acidosis if present.
- Cardiac catheterization may be done to determine cardiac functtioning.
Surgical Management
Surgery is a primary form of correction for CHDs, given their nature. Heart surgeries may be open or closed. Open heart surgeries operate on the idea that hypothermia will reduce O₂ consumption and allow for cardiopulmonary bypass, allowing for a bloodless field preventing bleeding and facilitating repair.
Palliative Management
Especially for tetralogy of fallot (TOF) and transposition of great arteries (TGA), palliative care is provided to improve oxygenation and circulation.
- TOF: - Blalock Taussig Anastomosis: the connection of the subclavian artery and pulmonary artery. - Potts Procedure: anastomosis of the aorta and pulmonary artery - Brock Procedure: the correction of pulmonary stenosis, but not the ventricular septal defect.
- TGA: - Blalock Hanlon: enlargement of the foramen ovale to improve flow. - Rashkind Procedure: an interatrial balloon septostomy. - Prostaglandin Infusion: maintains the patent ductus arteriosus and prevents it from closing.
Other Pediatric Diseases
- Respiratory Infections: 1. Bronchiolitis (viral infection) 2. Respiratory Syncytial Virus, manifested by expiratory wheezing
- Croup/Acute Laryngotracheobronchitis: can be viral or bacterial, manifested as inspiratory stridor. 1. Acute Infectious Laryngitis 2. Acute Spasmodic Laryngitis 3. Acute Laryngotracheobronchitis 4. Acute Epiglottitis (never depress the tongue as this may cause complete airway obstruction)
Fun Facts
(things the lecturer mentions, but is questionably within the scope of the presentation)
- Neonates primarily breathe through their nose, as adults do. This is why suctioning is done on the mouth first, before the nose.
- Failure of the neonate to breathe within 60 seconds
- Bilirubin is not produced by the liver; the liver produces glucuronyl transferase that converts indirect bilirubin to direct bilirubin. In newborns, this enzyme is not sufficient, which results in physiologic jaundice.
- The four signs of infection are rubor, tumor, calor, and dolor; respectively, redness, swelling, heat, and pain.
- Colostrum may begin begin produced as early as 5 months of pregnancy.
- Milk expressed during breastfeeding may be divided into two categories: foremilk and hindmilk. Foremilk contains more water and nutrients, while hindmilk contains more fat and calories. This is why it is important to perform complete breastfeeding.