This discussion is lifted from Ma'am Tuiza's presentation on Blood Transfusion (1 and 2). It will be supplemented with Kozier and Erb's Fundamentals of Nursing sometime soon.
A Blood Transfusion is the introduction of whole blood or other blood components into venous circulation. It is used to restore blood volume and the oxygen carrying capacity of the blood.
Blood Groups
As many know, different individuals have different blood groups. Blood typing involves two different factors: the antigens present on the red blood cells (and antibodies present in the plasma), and the presence of a rhesus (Rh) factor.
Antigens and Antibodies
Antigens are agglutinogens, and are present on the surfaces of the red blood cells. They dictate the blood type of the individual. These may be A, B, AB, and (if both are absent), O.
Antibodies are agglutinins, and are present in the plasma of an individual. They are normally the inverse of the antigens present in the blood. Otherwise, a rapid hemolytic reaction would occur, known as ABO- Incompatibility.
| A | B | AB | O | |
|---|---|---|---|---|
| Antibodies in Plasma | Anti-B | Anti-A | None | Anti-A and Anti-B |
| Antigens on RBC | A antigen | B antigen | A and B antigen | None |
| Can Transfuse From | A, O | B, O | AB, A, B, O | O |
| Can Transfuse To | A, AB | B, AB | AB | O, A, B, AB |
- O: the universal donor
- AB+: the universal recipient
A Rhesus (Rh) Factor is another protein possibly found on the surface of red blood cells, as discovered by Karl Landsteiner and A.S. Weiner in 1940. They may be present (Rh+) or absent (Rh-). The being Rh positive or negative has no bearing on health, except in the case of an Rh- mother bearing an Rh+ fetus. The leakage of Rh+ fetal blood during delivery can result in the development of Rh antibodies by the mother, which can attack subsequent the red blood cells of Rh+ fetuses. This is known as an Rh Incompatibility.
Blood Typing and Crossmatching
Blood Typing is done to determine the ABO blood group and Rh Factor status of an individual. This data is used to determine the blood transfusion options an individual has when the need for one arises.
Crossmatching is a test to determine the possible interactions of minor antigens with their corresponding antibodies: transfusion blood, recipient serum, and Coombs’ serum are all mixed to determine if agglutination will occur. If not, the risk of a transfusion reaction is small.
Blood Donation
Donors are not permitted to donate blood if they have any of the following:
- Hepatitis B, Hepatitis C, or HIV, or even just the risk factors for an HIV infection, disqualifies an individual from donation, as these can be transmitted by the blood.
- Heart Disease
- Most types of cancer
- Severe asthma
- Bleeding disorders, as venipuncture can result in excessive risk for the donor.
- Seizures
Some more definitions can defer donation; these are conditions that have to abate before donation:
- Malaria, or exposure to malaria or hepatitis.
- Anemia
- Abnormal blood pressure, both for high and low blood pressure
- Pregnancy
- Recent surgery
- Some types of medication
- 12 months after having a tattoo or piercing
Blood and Blood Products
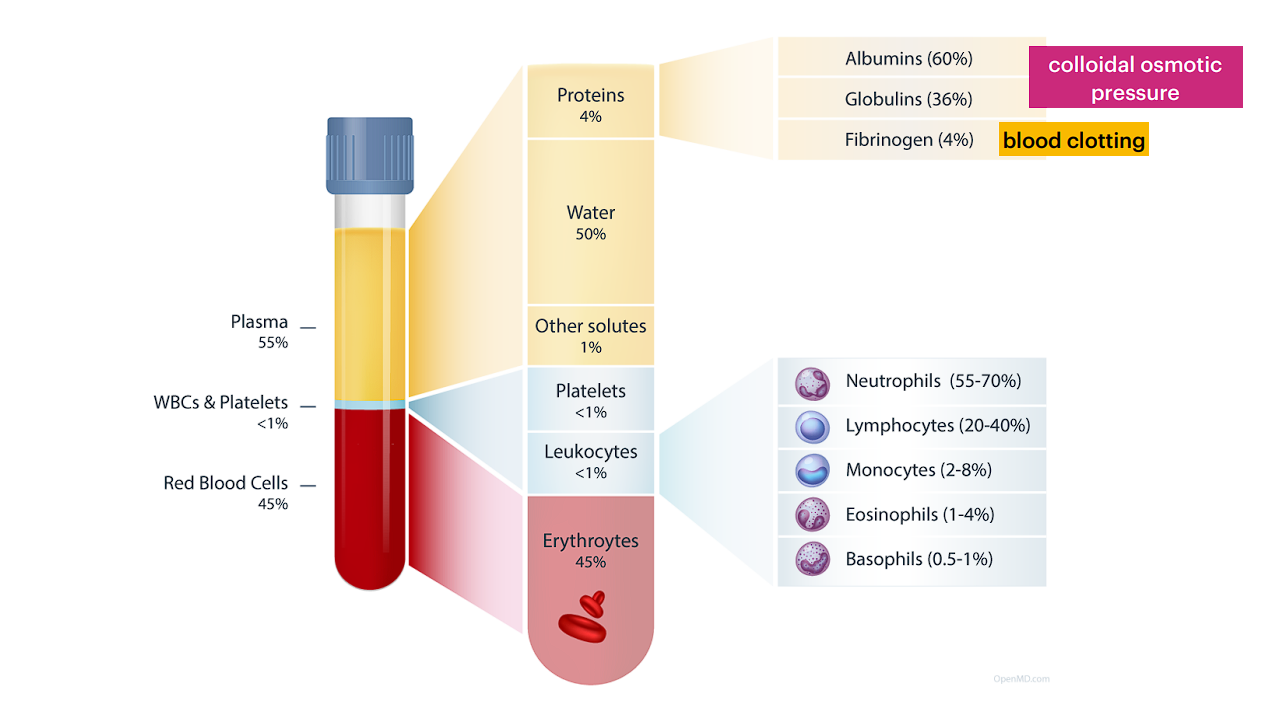
Blood is a stew of various cells, water, proteins, and other solutes. Here’s a diagram displaying more specific details:
 Blood transfusions don’t always use whole blood. Some patients only require components of the blood, and for different purposes. Here are some following blood products and their use-cases
Blood transfusions don’t always use whole blood. Some patients only require components of the blood, and for different purposes. Here are some following blood products and their use-cases
| Blood Product | Indications |
|---|---|
| Whole Blood | For extreme cases of acute hemorrhage: all blood products and volume are restored (RBC, Plasma, Protein, Platelets, Clotting Factors) |
| Packed RBCs (PRBCs) | For increasing oxygen-carrying capacity, such as in anemia, surgery, and slow bleeding disorders. In terms of units, PRBCs increase hematocrit by approximately 2% to 3%. The increase in oxygen carrying capacity in one unit is the same as in one unit of whole blood. |
| Autologous RBCs | For blood replacement following planned elective surgery. Autologous means the blood donor and receiver is the same individual. Donation is done 4 to 5 weeks prior to surgery. |
| Platelets | For bleeding disorders or platelet deficiency. Fresh platelets are the most effective. One unit of platelets increases platelet count by ~5,000 platelets per microliter. |
| Fresh Frozen Plasma | Provides clotting factors. The absence of RBCs means there is no need for typing and crossmatching when transfusing FFP. |
| Albumin and Plasma Protein Fraction | For volume expansion and plasma proteins. Albumin increases serum colloidal pressure, pulling fluid into circulation on top of its own volume. |
| Clotting Factors and Cryoprecipitate | For clotting factor deficiencies. Cryoprecipitate also helps with clotting as it contains fibrinogen. |
1 unit of whole blood is 500 mL; 1 unit of PRBC is 200 to 250 mL.
Administering Blood
Administering blood is a dependent nursing action. Blood is a delicate product, and requires strict storage, preparation, and administration guidelines to remain viable:
- Storage: blood is not stored at the nursing unit. The temperature control required for blood is greater, warranting its own storage system.
- Period of Viability: a blood bag, once removed from storage, should not hang for more than four hours. Any longer and the blood is at heightened risk of bacterial proliferation from being at room temperature. Prior to starting the transfusion, the bag must not be left in room temperature for more than 30 minutes for the same reason. If unexpected delays occur, the bag may be returned to the blood bank.
- IV Needle Gauge: traditionally, gauges #18 (green) to #20 (gray) were used for infusion. These are large-bore gauges that minimally restricts the flow rate of blood to prevent hemolysis. In current practice guidelines, #20 (pink) to #24 (yellow) is acceptable for transfusions in adults.
#14 (orange) to #18 (green) gauge may be used if rapid transfusion is required.
- Administration Set: Y-Sets or Piggyback Lines are used. Blood is not transfused by itself; a Y-set allows the vein to be kept open with normal saline while starting or ending the transfusion. The only solution compatible with blood or its components is normal saline (NSS).
- A new set is used for every component or every four hours. New IV tubing is used for administering other IV fluids following transfusion.
Handling a Y-Set
First and foremost, assess the patient. Obtain baseline vital signs and blood count (hemoglobin, platelet) and inspect the infusion site for its status and patency of the vascular access device used. A physical exam is done, especially for heart and lung sounds.
Next, plan for the transfusion: check for allergies, previous blood transfusions, the doctor’s order for the transfusion, written consent, and prepare the pre-transfusion medications (acetaminophen, diphenhydramine), usually 30 minutes before the actual transfusion.
Implementing the order requires the assistance of another RN: the best practice is to have one nurse read the information to the other nurse for verification. Both nurses verify the following information:
- The order for transfusion
- The transfusion consent form
- Client identifiers: obtain the patient name and identification number, identification band, compared to the name and number attached to the unit of blood.
- Unit identifiers: check the unit identification number on the blood container, the transfusion form, and the tag attached to the unit. All of them must comply with one another.
- Blood type: the ABO group and Rh type is placed on the label of the donor unit. This must be cross-referenced with the transfusion form.
Discrepancies
Any discrepancies should be reported to the charge nurse and blood bank. No administration of blood can be done until these discrepancies are corrected or clarified.
Monitoring: the patient is monitored for the first 15 minutes after the transfusion begins. The rate of transfusion should be slow (2 mL/min) during this period, to mitigate any possible reactions. After 15 minutes, the transfusion rate is increased if there are no reactions observed. Intermitted monitoring continues as follows (also depends on agency protocol):
- Check vital signs every 15 minutes for an hour, then every 30 minutes for an hour, then every hour for two hours.
- Rate of Transfusion: most adults are able to tolerate one unit of blood infused within 90 to 120 minutes. Again, transfusion must not exceed four hours.
- In case of an adverse reaction: the transfusion is halted, and sent back to the laboratory for investigation of the blood.
- Completion: if no infusion is to follow, the blood tubing is clamped. Depending on agency protocol, the blood bag is either returned or disposed in a biohazard container.
Finally, document the transfusion. This includes the date, time, procedure, assessment cues from before and after the transfusion, and any variances or observations.
Transfusion Reactions
There are five general transfusion reactions, related to hemolysis, anaphylaxis, circulatory overload (TACO, and lung injury (TRALI). These often occur within the first 15 minutes of transfusion (hence the continuous monitoring done during this period) or the first 50 ccs of blood transfused.
Acute Hemolytic Transfusion Reaction (AHTR) results from an incompatibility, resulting in the destruction of transfused RBCs, and kidney damage or failure.
- Clinical Signs: fever/chills, flank/back pain, reddish or brown urine (hemoglobinuria), hypotension, tachycardia, apprehension (“sense of impending doom”)
- Intervention: discontinue immediately; vascular access is maintained with normal saline (or according to agency protocol). The physician is notified immediately and monitoring of the patient is begun. Vital signs and fluid intake and output are monitored. The blood, its bag, filter, tubing, and a sample of the client’s blood and urine are all sent to the laboratory.
Non-Hemolytic Febrile Reaction results from a sensitivity of the client’s blood to white blood cells, platelets, or plasma proteins. This reaction does not destroy red blood cells (non-hemolytic).
- Clinical Signs: fever, chills, warm flushed skin, headache, anxiety, nausea and vomiting
- Intervention: discontinue immediately; vascular access is maintained with normal saline (or according to agency protocol). The physician is notified immediately and antipyretics are given.
Allergic Reactions can occur and can range in severity, from mild to severe.
- Clinical Signs: (mild) flushing, urticaria (potentially non-pruritic); (severe) dyspnea, stridor, decreased SpO₂, hypotension, and shock.
- Intervention: discontinue immediately; vascular access is maintained with normal saline (or according to agency protocol). The physician is notified immediately and monitoring of the patient’s vital signs is begun. CPR may be necessary. Administer medications and oxygen as ordered.
Transfusion-Associated Circulatory Overload, or just circulatory overload, occurs when the rate of blood administration is faster than circulation can accommodate for.
- Clinical Signs: dyspnea, orthopnea, crackles (rales), distended neck veins, tachycardia, and high blood pressure.
- Intervention: discontinue immediately. The patient is positioned upright to improve breathing (orthopnea, lung edema). The physician is notified, and diuretics and oxygen are given as ordered.
Transfusion-Related Acute Lung Injury (TRALI) is an autoimmune response to infused donor leukocyte antibodies.
- Clinical Signs: acute respiratory distress, hypotension, hypoxemia, fever, chills
- Intervention: discontinue immediately; vascular access is maintained with normal saline (or according to agency protocol). The physician is notified immediately. Oxygen therapy is initiated, potentially with a mechanical ventilator. Hypotension is corrected with fluid resuscitation, and potentially with vasopressors if necessary. The remaining blood and tubing is sent back to the laboratory.