Read Also: Pancreas, Hypoglycemia, Hyperglycemia, Diabetic Ketoacidosis, Hyperglycemic Hyperosmolar Nonketotic Syndrome
Various metabolic disorders resulting in a characteristic hyperglycemia subsequent to deficiency and/or dysfunction of insulin may result in diabetes mellitus (DM).
Type 1 Diabetes (Insulin-Dependent)
Type 1 comprises approximately 5% to 10% of all diabetes cases. It is characterized by the destruction of pancreatic beta-cells due to genetic, immunologic, or even environmental factors. The primary intervention is insulin therapy. Its onset and development is rapid, often occurring before the age of 30.
Type 2 Diabetes (Non-Insulin-Dependent)
Type 2 comprises the remaining 90% to 95% of diabetes cases. It is a result of decreased sensitivity to insulin (insulin resistance) or decreased insulin production. Interventions start with dieting and exercise, then with hypoglycemic agents as necessary. It often occurs in obese patients, usually after the age of 30.
Gestational Diabetes Mellitus
Glucose intolerance develops during pregnancy (often in the second or third trimester). Risk factors include obesity, history of gestational diabetes, glycosuria, family history, and ethnicity (hispanic, american, native american, asian american, african american, pacific islanders). This often contributes to the hypertensive disorders of pregnancy.
Secondary Diabetes Mellitus
DM may also be a result of other conditions or syndromes e.g. pancreatic disease, Cushing’s syndrome, drug use (steroids, thiazide diuretics, oral contraceptions)
Assessment Findings
- Polyuria (osmotic diuresis), Polydipsia (secondary to polyuria), Polyphagia (due to ineffective utilization of glucose stores); the hallmark signs (3 Ps) of diabetes mellitus.
- Fatigue and weakness (ineffective utilization of glucose), sudden vision changes (diabetic retinopathy), tingling or numbness in hands or feet (peripheral neuropathy), dry skin (fluid shift d/t hyperglycemia), skin lesions (including diabetic ulcers) or wounds that heal slowly, recurrent infections.
- Onset of Type 1 Diabetes: sudden weight loss or nausea, vomiting, or stomach pains.
- Type 2 Diabetes: progressive glucose intolerance, which may result in eye disease, peripheral neuropathy, peripheral vascular disease) if undetected and unmanaged.
- Diabetic Ketoacidosis: abdominal pain, nausea, vomiting, hyperventilation, and a fruity breath odor. This may develop to include altered level of consciousness, coma, and death.
Diagnostic Examination
- Fasting Blood Sugar: after 8 hours of fasting; two tests resulting in 126 mg/dL or greater (normally 70 to 100 mg/dL). In between 100 and 126 is considered the prediabetic range.
- Random Blood Sugar: 200 mg/dL or greater combined with symptoms is suggestive of DM.
- Postprandial Blood Sugar: 2 hours after a high carbohydrate meal; 200 mg/dL or greater; <200 and >140 mg/dL is prediabetic, 70 to 140 mg/dL is normal.
- Oral Glucose Tolerance Test (OGTT)
- Three days of a high carbohydrate diet is followed by an 8 hour fasting
- A baseline blood sample and urine specimen is collected.
- The client takes an oral glucose solution
- Blood is drawn 30 minutes, 1 hour, 2 hours, and 3 hours after ingestion.
- Urine is collected.
- If blood glucose levels return to normal slowly and urine is positive for glucose, DM is suggested.
- Glycosylated Hemoglobin (HbA1c): a sample of venous blood is drawn, and HbA1c, the form hemoglobin takes when combined with glucose, is elevated at above 7% in patients with undetected, untreated, or inadequately treated DM (or they are non-compliant to therapy).
- Evaluation for complications
Prevention
- For obese patients (especially those with Type 2 DM), weight loss is key to treatment. It is also the major preventive factor for the development of diabetes.
Complications
There are three major acute complications of DM:
- Hypoglycemia
- Diabetic Ketoacidosis (DKA) as a result of compensatory protein and fat breakdown in lieu of inadequate glucose utilization. Commonly found in Type 1 DM.
- Hyperglycemic Hyperosmotic Nonketotic Syndrome (HHNS), a syndrome that results in high blood pressure. Commonly found in Type 2 DM.
Long term complications include:
- Microangiopathy
- Renal failure from nephropathy
- Cataract formation due to retinopathy
- Macroangiopathy
- CADs like MI, CVAs, and Peripheral Vascular Disease
- Neuropathy
- Spinal cord, ANS
- Peripheral Neuropathy: damage to the PNS, affecting movement, sensation, and bodily functions; paresthesia
- Gastroparesis: delaying of gastric emptying.
- Neurogenic Bladder: inappropriate emptying of the bladder.
- Decreased Libido and Impotence
Gerontologic Considerations
Blood glucose levels normally elevate with advancing age. Elderly adults should be advised that physical activity that is consistent and realistic is beneficial to those with diabetes. Consider physical impairment from other chronic diseases when planning exercise regimens for elderly patients with diabetes.
Medical Management
The main goal is to normalize insulin activity and to maintain normal blood glucose levels, reducing resultant vascular and neuropathic complications. There are five components in therapy: nutrition, exercise, monitoring, pharmacology, and education.
- Type 1: insulin replacement
- Type 2: weight reduction
- General: diet and exercise improves insulin sensitivity; if still unmanageable, oral hypoglycemic agents are used. Insulin injections may be used in acute situations.
- Exercise should be done 1 to 2 hours after eating to prevent hypoglycemia.
- Exercise should be done with a schedule; non-sporadically.
Insulin Therapy
Insulin may be sourced from pork, beef, and human sources. Human insulin has the lowest incidence of hypersensitivity reactions. As such, it is recommended for all newly diagnosed Type 1 diabetics, short-term insulin therapy for Type 2 Diabetics, pregnant clients, and diabetic clients with hypersensitivity or severe insulin resistance.
| Insulin | Onset | Peak | Duration |
|---|---|---|---|
| Rapid Acting (Clear): Lispro (Humalog), Aspart (Novalog) | 5 mins | 30 to 60 mins | 2 to 4 hours |
| Short Acting (Clear): Regular (Humulin R, Novolin R, Iletin II regular) | 30 to 60 mins | to 4 hours | 6 to 8 hours |
| Intermediate (Cloudy): NPH | 1 to 2 hours | 6 to 12 hours | 18 to 24 hours |
| Intermediate (Cloudy): Humulin N Lente | 1 to 2 hours | 8 to 12 hours | 18 to 24 hours |
| Intermediate (Cloudy): Humulin L | 1 to 2 hours | 8 to 12 hours | 18 to 28 hours |
| Long Acting: Ultralente Glargine (Lantus) | 5 to 8 hours | 14 to 20 hours | 30 to 36 hours |
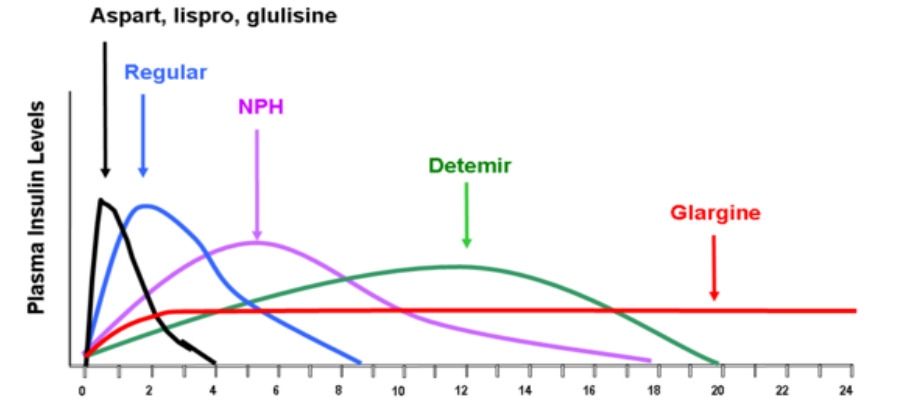 |
Oral Hypoglycemia Agents
Often used for Type 2 Diabetics, these are generally divided between:
- Sulfonylureas: “insulin releasers” that stimulate beta cells to secrete more insulin. It also increases the ability of insulin receptors to bind to insulin.
- Side Effects: weight gain, hypoglycemia, pancreatic failure due to overstimulation
- Tolbutamide (Orinase), Acetohexamide (Dymelor), Tolazamide (Tolinase), Chlorpropamide (Diabenese), Glipizide (Glucotrol), Glyburide (Micronase, Glynase), Glimepiride (Amaryl)
Alcohol Intake with Sulfonylureas can cause hyperemesis!
- Nonsulfonylureas
- Biguanides
- Metformin (Glucophage): helps tissues use available insulin more efficiently; insulin (receptor) sensitizers.
- Side Effects: upset stomach, flatulence, diarrhea
- Metformin (Glucophage): helps tissues use available insulin more efficiently; insulin (receptor) sensitizers.
- Alpha-glucosidase inhibitors
- Miglitol (Glyset), Acarbose (Precose): glucose formation from digestion is inhibited. Taken 15 minutes before meals to decrease duodenal absorption of glucose.
- Thiazolidinediones
- Rosiglitazone (Avandia), Pioglitazone (Actos): same as biguanides
- Side Effects: weight gain, edema, liver damage (monitor SGPT)
- Rosiglitazone (Avandia), Pioglitazone (Actos): same as biguanides
- Meglitinides
- Repaglinide (Prandin): an insulin releaser
- Side Effects: same as sulfonylureas
- Repaglinide (Prandin): an insulin releaser
- Biguanides
Nutritional Management
- Low caloric diet for obese patients with 50-20-30 CPF ratios. CHO should be complex, and fiber should be high; this inhibits glucose absorption in the intestines.
- Maintain blood sugar
- Maintain blood pressure
- Maintain blood lipids and lipoproteins
- Maintain the pleasure of eating; consider preferences, lifestyle, schedule, and culture.
- Slow the progression of chronic complications
Nursing Management
- Client education should involve adherence, importance of consistent healthy eating habits, nature of the disease, and dietary management skills (reading food labels, creating and adjusting meal plans, exercise, etc.), and insulin therapy
- Monitor urine sugar and acetone.
- Monitor blood glucose
- Provide skin and oral care. Perform good oral hygiene.
- Regular check-up every 3 months, regular dental exams, regular eye exams
- Maintain I&O, weigh daily
- Observe for chronic complications
Nursing Responsibility: Insulin Therapy
- Insulin is normally administered subcutaneously (90° for thin patients, 45° for obese clients). This route is less painful and facilitates slower absorption of the administered dose. No need to aspirate, do not massage.
- Intravenous Insulin may be used for emergency cases such as in DKA.
- Insulin should be administered at room temperature. The vial of insulin being used should be kept at room temperate. It can be kept like so for a month. Other vials not currently being used should be refrigerated.
- Cold insulin results in lipodystrophy; lipoatrophy often from animal insulin or lipohypertrophy (fibrofatty masses) from repeated use of a site. This also prevents proper absorption of insulin. Prevent lipohypertrophy by rotating sites of administration.
- Roll the vial of insulin between the palms to redistribute insulin particles, but do not shake it. Bubbles cause difficulty in aspirating exact amounts.
- Observe for Side Effects:
- Local: induration, redness, swelling, lesion formation, lipodystrophy
- Generalized: edema formation (acute resolution of hyperglycemia results in ECF shift), hypoglycemia (rebound), somogyi phenomenon (rebound morning hyperglycemia from late-night hypoglycemia)
- Insulin may also be delivered via an Insulin Pump. A computer manages a continuous dosage throughout the day, closely mimicking pancreatic function. It administers subcutaneously via a needle or teflon catheter connected to a 42-inch narrow lumen tube containing 3 ml of regular insulin. It is usually placed on the abdomen and attached to a belt or pocket.
- Basal rate: often 0.5 to 2 units per hour
- Bolus dose: administered before meals
Pathophysiology
Polyuria, Polydipsia
flowchart TB
1A("Stress")
1B("Diabetes Mellitus")-->2
1A--"Stress Response"-->2
2("Hyperglycemia")
3A("High Osmotic Pressure\nin Renal Tubules")
3B("High Blood\nOsmolarity")-->4B("ICF Dehydration")-->4A
3C("Breaking renal threshold\n(>180 mg/dL blood sugar)")
4A("Polyuria")
4C("Glycosuria")
2-->3A
2-->3B
2-->3C
3A-- Osmotic Diuresis -->4A
4A-->5("Polydipsia")
4A-->6("ECF Dehydration")
3C-->4C
Polyphagia, DKA, CVD, Wasting
flowchart TD
A(Underutilized Blood Glucose)-->B(Cellular Starvation)
B-->C(Polyphagia)
B-->D(Lipolysis)
B-->E(Gluconeogenesis)
D-->D1(Ketone Production)
D1-->D2(Ketonemia)
D1-->D3(Ketouria)
D2-->D4("Metabolic\nAcidosis")
D3-->D5("Polyuria")
D-->F1("Hyperlipidemia")
F1-->F2("Atherosclerosis")
F2-->F3("Cardiovascular Disease")
subgraph " "
E-->E1("(-) Nitrogen Balance")
E1---E2("Tissue Wasting")
E2---E3("Weight Loss")
E3---E4("Debilitation")
end
Decreased Blood Viscosity
flowchart TB
A1(Dehydration)
A2(Increased Serum Osmolality)
A1-->B(Increased Blood Viscosity)
A2-->B
B-->C1(Sluggish Circulation)
B-->C2(Proliferation of Microorganisms)
Microorganism proliferation results in infections, periodontal disease, UTI, vasculitis, cellulitis, vaginitis, furuncles, carbuncles, and retarded wound healing. Feet must be inspected and cleaned daily to prevent a diabetic foot.