Anatomy of the Ear Surface
Anatomy and Physiology of the Ear
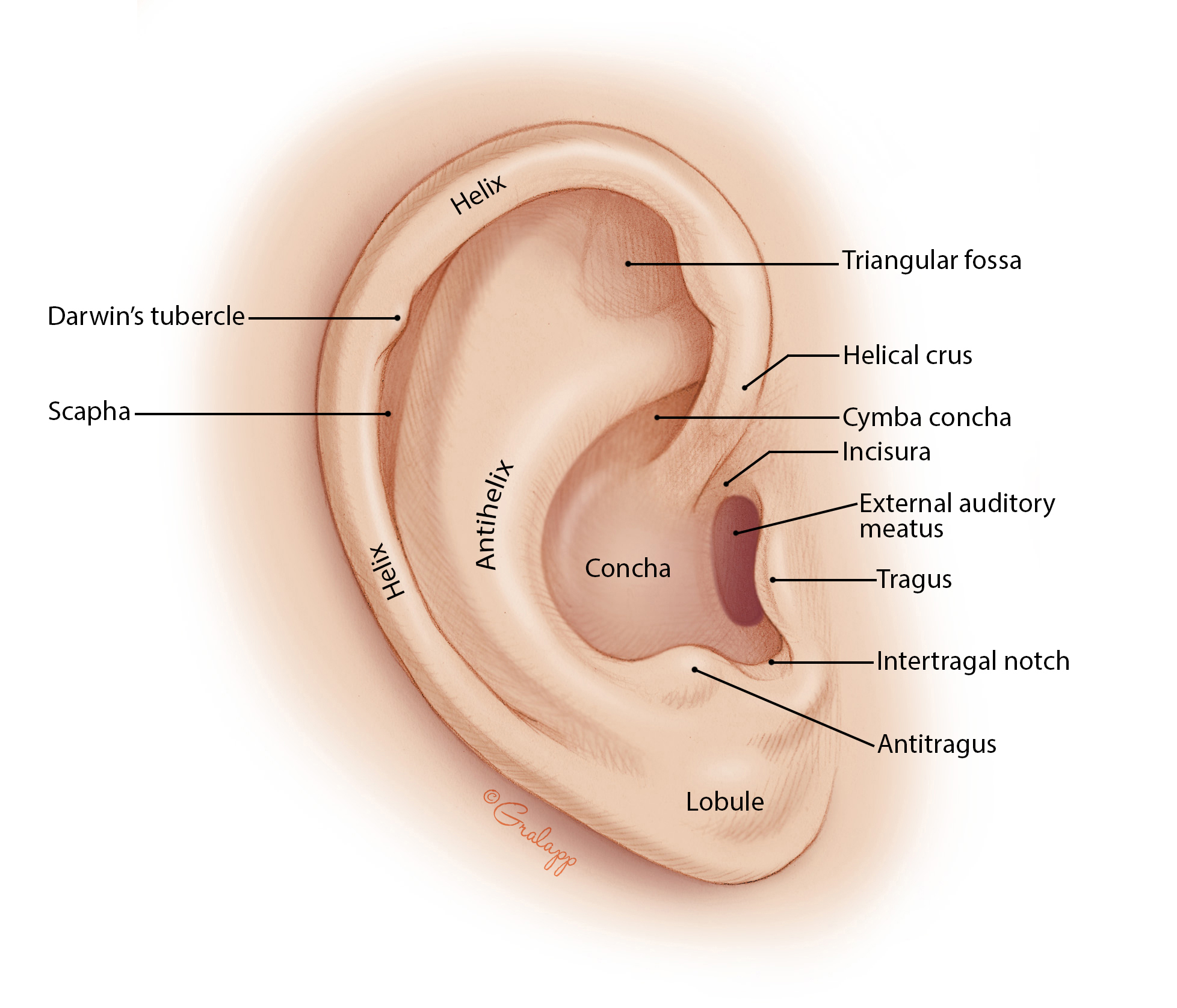
External Ear
The external ear consists of the auricle (pinna) and external auditory canal (ear canal). This region collects sound waves and directs them to the middle portion of the ear.
- Auricle, also known as the pinna, is a cartilaginous outer “funnel” that collects sound waves into the ear canal. This part is mainly made of cartilage (except for fat and subcutaneous tissue in the ear lobe).
- This is the part of the ear manipulated during Otoscopy and Otic Medication Administration
- External Auditory Canal, also known as the ear canal, is an approximately 2 to 3 cm long canal that ends at the tympanic membrane. This contains hair, sebaceous glands, and ceruminous glands (where ear wax, cerumen, comes from), which normally slowly clears the ear of debris and old cerumen. This may become impacted.
- Just anterior to the external auditory canal is the temporomandibular joint, whose head can be felt by placing a fingertip in the external auditory canal while the patient opens and closes their mouth.
Disorder
- An erythematous ear canal indicates Otitis Externa, inflammation of the ear canal.
- The ear canal is normally skin colored. If inflamed, it is erythematous.
- Aural tenderness occurs, where manipulation of the pinna, oracle, or canal causes pain.
- Treatment: analgesics (otic drops)
Middle Ear
The middle ear is an air-filled cavity, and includes the tympanic membrane/tympanum (eardrum), eustachian tube, the ossicles. The ossicles (malleus, incus, stapes) end at the oval window, which is what separates the middle ear from the inner ear.
- Tympanic Membrane: the structure separating the external ear from the middle ear. It is a thin, translucent, pearly gray membrane that protects the middle ear and conducts sound vibrations from the external canal to the ossicles.
- Ossicles: the three smallest bones of the body: malleus (hammer), incus (anvil), stapes (stirrups), connected by joints, muscles, and ligaments, conduct vibrations to the oval window, which separates the inner ear from the middle ear. Another fenestra, the round window, also on the border between the middle and inner ear, and acts as an exit point for the pressure waves.
Disorder
- Problems with the external or middle ear that results in hearing loss is conductive hearing loss.
- In otitis media, the tympanic membrane bulges and becomes erythematous (normally pearly grey).
- URTIs travelling through the eustachian tube can produce Otitis Media. In children, this tube is smaller, and more easily transfers infective agents.
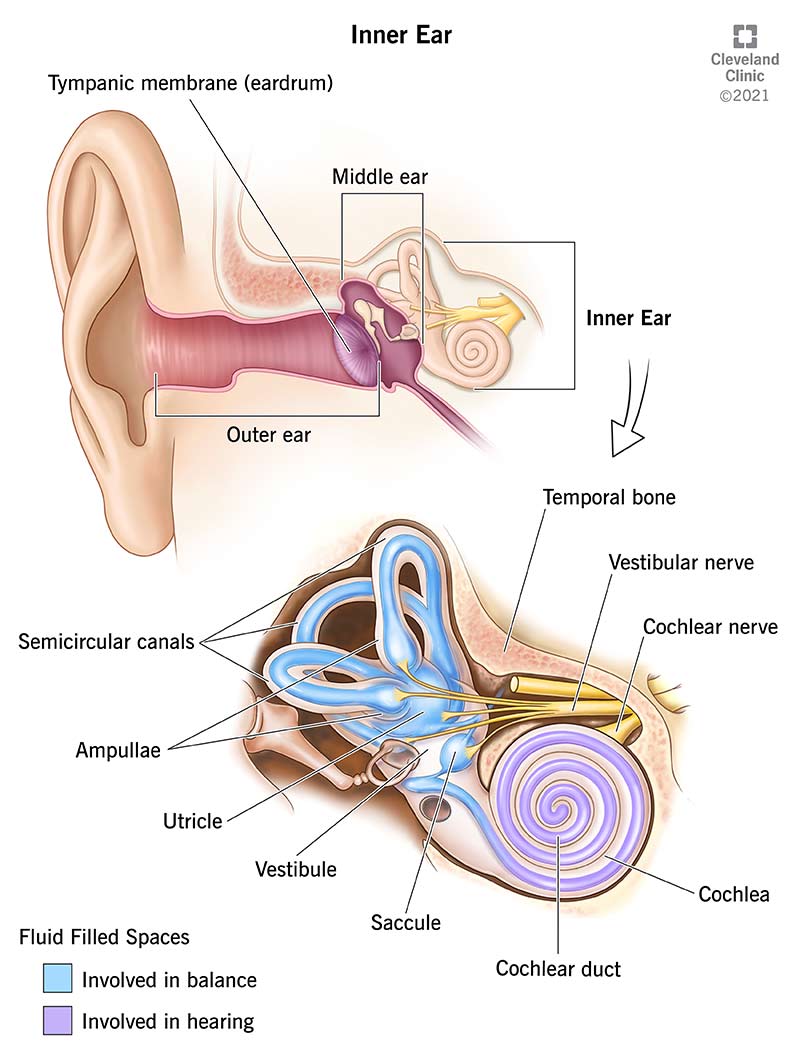
Inner Ear
The inner ear is housed within the temporal bone. The organs for hearing (Cochlea), and balance (Semicircular Canals), as well as CN VII (Facial) and CN VIII (Vestibulocochlear). The cochlea and semicircular canals are housed in the Bony Labyrinth, which houses the Membranous Labyrinth. It is filled with endolymph and surrounded by perilymph. This fluid helps with the conversion of mechanical energy into neural impulses. The oval window connects to the vestibule, which is connected to both the semicircular canals responsible for balance, and the cochlea, responsible for hearing.
- Membranous Labyrinth: composed of the utricle, the saccule, the cochlear duct, the semicircular canals, and the Organ of Corti, all of which are surrounded by endolymph, a fluid.
- Semicircular Canals: there are three (posterior, superior, lateral) which lie at 90-degree angles to one-another. They contain sensory receptor organs that are arranged to detect rotational movement. These receptor end organs are stimulated by changes in the rate or direction of a person’s movement.
- The utricle and saccule are involved in linear movement. The utricle is horizontal-lying, and detects horizontal motion. The saccule is vertical, and detects motion along the sagittal plane; up, down, front, back.
- Organ of Corti: is the end organ for hearing. It is housed in the cochlea, a snail-shaped, bony tube about 3.5 cm long with two and a half spiral turns. It is located in the basilar membrane.
Disorder
- Labyrinthitis.
- Problems with the inner ear or labyrinth that results in hearing loss is sensorineural hearing loss. Often caused by (mn. LMP) labyrinthitis, Meniere’s syndrome, and Presbycusis.
Physiology of Hearing
- The auricle (pinna) “gathers” sound waves, and redirects them to the external auditory canal and to the eardrum.
- The tympanum vibrates, sending vibrations across the bridge of ossicles, which connects with the oval window.
- The oval window vibrates as the stapes/stirrups strikes it, and vibrates the fluid within the vestibule.
- A round window lies further in the inner ear, and acts as a pressure valve; it bulges out when the inner ear pressure becomes elevated.
- The sensitive part of the inner ear, the Organ of Corti, functions as the body’s microphone with miniscule hairs that move with the endolymph’s waves. It is situated in the basilar membrane of one of the three components of the cochlea.
- The Vestibulocochlear Nerve, CN 8 (Read also: cranial nerve), facilitates hearing and equilibrium. The nerve fibers arise from the hearing and equilibrium apparatus of the inner ear, pass through the internal acoustic meatus, and enters the brainstem at the pons-medulla border. There are two divisions of this system: the cochlear (hearing) and vestibular (balance; equilibrium). CN 8 demonstrates purely sensory functions. The Facial Nerve, CN 7, innervates the stapedius muscle, which places tension on the bones of the middle ear. This tension regulates sound and protects the inner ear from damage due to loud sounds.
- The auditory cortex in the cerebrum then receive the impulses and decodes them as experienced sounds.
Functions of the Ear
- Hearing is the most basic function of the ear. Vibrations are interpreted as sound in the brain after being transmitted and transformed into nerve signals by the cochlea. This process may be done with air conduction (air-filled external and middle ear through vibration of the tympanic membrane and ossicles) or bone conduction, where the vibrations travel through bone and the inner ear, bypassing the tympanic membrane and ossicles. Air conduction is normally efficient at detecting vibrations.
- Sound Conduction and Transmission: sound enters through the (1) external auditory canal, and causes the (2) tympanic membrane to vibrate. The (3) ossicles, through lever action, transmit the sound as mechanical energy into the (4) oval window, transmitting it through the (5) inner ear fluids (perilymph, endolymph) to the (6) cochlea, stimulating (7) hair cells, converting the mechanical energy into electrical energy. These travel through the (8) vestibulocochlear nerve (CN VIII) to the (9) central nervous system, where it is interpreted.
- Sound conduction is impeded in a perforated tympanum, as this allows sound waves to apply pressure on the round window, which is normally an exit point for pressure waves.
- Balance is another important function. There are three semicircular canals in the inner ear. They are oriented at right angles to each other, and the resulting differences in the fluids of the canals helps the brain identify or detect the extent of movement and positioning of the head.
- Balance is achieved with the cooperation of muscles and joints in the body (proprioceptive system), the eyes (visual system), and the labyrinth (vestibular system). Each system informs the cerebellar system in the cerebral cortex about the body’s equilibrium for coordination and perception in the cerebral cortex. These, including the cardiovascular system that supplies the brain with blood, when damaged, all contribute to disturbance of balance.
Assessment of the Ear
The ears are located on either side of the cranium at approximately eye level. Assessment involves inspection of the external, middle, and inner ear. Gross hearing acuity is also measured in every physical examination.
External Ear
While simple, this is often overlooked. The external ear consists of the auricle (pinna) and the external auditory canal, and is separated from the middle ear by the tympanic membrane. Utilize inspection and direct palpation for assessment.
- Inspect and palpate the auricle and surrounding tissues for masses, lesions, deformity, and placement, as well as size, symmetry, and angle of attachment to the head.
- Move the auricle and press on the tragus to check for pain. Manipulation normally does not produce pain. If so, acute external otitis is suspected.
- Tenderness of the mastoid may indicate acute mastoiditis or inflammation of the postauricular node.
- Assess for discharge from the ear.
- Occasionally, sebaceous cysts and tophi form on the pinna. A flaky scaliness on or behind the auricle usually indicates seborrheic dermatitis and can be present on the scalp and facial structures as well.
Internal Ear
Assessment of the inner ear requires Otoscopic Examination (sometimes inverted).
- Ear Canal: normally pink and intact.
- Cerumen (ear wax) is normal to an extent, but may become impacted; Impacted Cerumen.
- Check for Erythema and Edema
- Check for Tenderness
- Tympanic Membrane: normally pearly gray, semi-transparent, and intact. With partial transparency, some inner structures may be visible like the long process of the incus and the opening of the eustachian tube. The handle of the malleus, which extends downwards and backwards, is a reliable landmark.
Gross Auditory Acuity (Hearing Assessment)
Whisper Test
Test hearing acuity.
- Procedure: stand 1 to 2 feet to the side or behind the patient. Instruct the patient to obstruct the contralateral ear. The nurse whispers words with two distinct syllables (e.g., baseball, cellphone, pencil), and asks the patient to repeat the words spoken. They should be able to repeat the spoken words. This is done for both ears.
- Interpretation: if the patient is able to repeat the words, they pass. Failure requires more specific assessments and Audiometry.
Weber Test
This test differentiates conductive from sensorineural hearing.
- Procedure: strike a (512 Hz, ideally) tuning fork softly, and place it on the patient’s head (on top, or by the forehead).
- Interpretation: Ask the patient if they hear the sound on both sides equally. This is normal, and the patient may describe it as “inside their head”. If the sound undergoes “lateralization”, it is abnormal. If the sound is stronger on the “poor” ear, then it demonstrates conductive hearing loss. If it is stronger on the good ear, then it demonstrates sensorineural hearing loss. Sensorineural hearing loss manifests as the sound being heard better in the normal ear, because the bypassed conductive parts of the ear did not impact the patient’s ability to hear. If conductive hearing loss is present, then bypassing them with bone conduction allows the patient to hear better in the otherwise-affected ear.
| Result | Interpretation |
|---|---|
| Heard midline/equally on both sides | Normal |
| Lateralization towards the Affected Ear | Conductive Hearing Loss |
| Lateralization towards the Unaffected Ear | Sensorineural Hearing Loss |
Rinne Test
This test compares air and bone conduction to identify conductive or sensorineural hearing loss.
- Procedure: the same process as Weber, but the base of the tuning fork is placed on the mastoid bone (for bone conduction). Ask them to state when the sound is no longer heard (note the duration/time interval). Repeat the test, but while holding the tuning fork next to the auditory meatus, about two inches away (for air conduction). Alternatively, allow the patient to identify which “sounds louder” instead of using time.
- Interpretation: Ask them to state when the sound is no longer heard (note the duration/time interval). Normally, the patient should hear air conduction better than and longer than bone conduction, and this is documented as a positive Rinne test. In conductive hearing loss, bone conduction is better heard than air conduction (same or longer time interval), and is documented as a negative Rinne test. If the patient displays hearing loss, but air conduction remains superior to bone conduction, suspect sensorineural hearing loss.
| Result | Interpretation |
|---|---|
| Air Conduction is louder/lasts longer than Bone Conduction | (+) Positive; Normal |
| Air Conduction is shorter than or equal to Bone Conduction | (-) Negative; Conductive Hearing Loss |
| Air Conduction is louder/lasts longer than Bone Conduction | (+) False Positive; Sensorineural Hearing Loss |
Diagnostic Examination of the Ear
Otoscopic Examination
The tympanic membrane is inspected with an otoscope and indirect palpation with a pneumatic otoscope. With the right hand holding the otoscope in a pen-like fashion, and the other hand braced against the patient’s face, the largest speculum usable (normally 5 mm for adults) is gently guided down into the canal and forward. The distal portion of the canal contains thin, sensitive skin, and produces pain when pressure is applied.
- Straighten the external auditory canal by pulling the pinna (in an adult) backwards and upwards, or (in a child) backwards and downwards.
- Examine for discharge, inflammation, or Foreign Bodies.
- The position and color of the membrane, and any unusual markings, deviations, (and in the middle ear, through the semi-transparent tympanum) fluid, air bubbles, blood, or masses are all noted.
- Obstruction by cerumen calls for cerumen removal through various methods discussed under Cerumen Impaction. However, small amounts are normal and should not be interfered with.
- The healthy tympanic membrane is pearly gray and positioned obliquely at the base of the canal.
Audiometry
The single most important test for detecting hearing loss; also known as audiography or an audiogram. It tests a person’s ability to hear various sound frequencies and measures hearing acuity. It uses an audiometer used by an audiologist, a trained technician. There are two types of audiometry: Pure-Tone Audiometry, which plays a single tone played quietly and increased in volume until heard by the patient, and Speech Audiometry, where spoken words are used to determine the ability to hear and discriminate sounds and words.
- No special precautions required. The patient sits in a soundproof chamber or cubicle, puts on headphones, and signals to the examiner when they can hear the stimulus. Conductive hearing is measured by tones directed over the external auditory canal, and nerve conduction is measured by tones directed onto the mastoid bone.
- Otoscopy may be done prior to audiometry testing to determine if any blockages are present (foreign body, cerumen).
- Normal hearing in adults can detect sounds from 20 to 20,000 Hz in frequency (Speech Frequencies span from 500 to 2,000 Hz) played as softly as 0 to 20 dB, and speech from 20 to 50 dB in volume. Anything over 80 dB may be perceived as harsh and injurious to the inner ear.
- The important level of loudness is ~30 dB, within the speech frequencies (500 to 3,000 Hz), and it is the goal of hearing-improvement surgery.
- Inability to hear pure tones below 25 dB indicate some extent of hearing loss.
| Loss in dB | Interpretation |
|---|---|
| 0-15 | Normal Hearing |
| 15-25 | Slight hearing loss |
| 25-40 | Mild hearing loss |
| 40-55 | Moderate hearing loss |
| 55-70 | Moderate to severe hearing loss |
| 70-90 | Severe hearing loss |
| >90 | Profound hearing loss |
Tympanometry
A test to check the condition and mobility of the ear drum, to detect disorders of the middle ear. It is an otoscopic exam that varies the air pressure in a sealed ear canal, and measures the ear muscle reflex responses to the pressure changes.
- Inform the patient to avoid speaking, moving, swallowing, or being startled (especially by the loud noises during examination), as these alter middle ear pressure and may invalidate test results.
Brain Stem Auditory Evoked Response (BAER)
Also known as Auditory Brain Stem Response (ABR) Audiometry. This test helps diagnose nervous system abnormalities, hearing losses (especially in LBW newborns), and to assess neurologic functions. Brain waves are stimulated in response to a clicking sound, which is used to evaluate the central auditory pathways of the brainstem.
- Patients may be asked to wash their hair the night before the test. Do not apply any additional products.
- Electrodes are placed on the patient’s scalp and on each earlobe, then acoustic stimuli (e.g. clicks) are made in the ear. Resultant electro-physiologic measurements can determine when the patient is able to hear (in dB) the stimuli, and any impairments along the nerve pathways (e.g., a tumor on the vestibulocochlear nerve).
Electronystagmography (ENG)
A vestibular test that evaluates electric potentials created by spontaneous, positional, or calorically evoked nystagmus. These record the electrical fields that occur with movements of the eye (the patient is instructed to follow a moving target; eye movements are monitored while the head is placed in different directions), and is used to determine causes of unilateral hearing loss, vertigo, or tinnitus.
- Damage to the nerve of the inner ear is one of the more common causes of vertigo.
- All vestibular suppressants (alcohol, caffeine, etc.) are withheld 48 hours before the exam. Anti-dizziness, anti-depressant, anti-histamine, tranquilizing, or sedative drugs or narcotics of any type are stopped 5 days prior to the balance test. These including codeine and medications containing codeine.
- Do not eat for 3 hours before the examination.
- Do not use facial creams or make up, as they may interfere with accurate recording during the test.
- Someone must accompany the patient to the test to drive them home, as dizziness is induced.
- The Caloric Test may be used to induce nystagmus. It involves stimulating the inner ear with temperature changes in order to test the nystagmus response. Warm or cold water or air is circulated in the ear canal. A normal response follows the COWS mnemonic: Cold, Opposite; Warm, Same side. The nystagmus moves contralateral to the instillation in cold water, and moves ipsilateral to the instillation if warm water is used. This movement is known as the vestibulo-ocular reflex.
General Care for Ear Surgeries
Pre-operative
- Assess for URTI.
- Shampoo the hair.
Post-operative
- Nose-blowing is to be avoided for a few weeks after surgery.
- Sneezing or coughing should be done with the mouth open for a few weeks after surgery.
- Heavy lifting, straining, and bending over are to be avoided.
- Lie on the unaffected side.
- Avoid physical activity for 1 week and exercise or sports for 3 weeks.
- Protect the ear with two pieces of cotton, with the outer piece being saturated with petrolatum. Change these cotton balls daily.
- Keep the ear dry for 6 weeks post-op,.
- Do not shampoo the hair for 1 week.
- Avoid airplane travel for 1 week. If ear pressure is felt, hold the nose shut, close the mouth, then swallow to equalize the pressure.
- Avoid reading, watching TV, or fast moving objects for 1 week post-op.
- Seek supervision when beginning to ambulate. Dizziness or lightheadedness may occur.
Hearing Loss
Hearing loss is reported in 0.2% to 0.3% of infants born in the U.S., with half of them being associated with a genetic sensorineural hearing loss (refer to pg. 1943 for associated genetic disorders). It may also be acquired: TORCH (Toxoplasmosis, Rubella, Cytomegalovirus, Herpes) infections during pregnancy, trauma, and chronic exposure to loud noise.
- Newborns are offered universal hearing screenings after birth and prior to discharge.
- Hearing loss occurs more in men than women. Approximately 2% of adults between the ages of 45 and 54 years have disabling hearing loss, 8.5% in 55 to 64 years, 25% in 65 to 74 years, and 50% over 75%. As people age, hearing screening and treatment are recommended.
- Noice-Induced Hearing Loss: occupational hazard (construction, plumbing, coal-mining, pilots, artillery workers, etc.
- Acoustic Trauma refers to hearing loss from a single exposure to an extremely loud stimulus.
- Conductive Hearing Loss often results from external ear disorders (e.g. Cerumen Impaction) or middle ear disorders (Otitis Media, Otosclerosis), where conduction of pressure waves fail to reach the organ of hearing effectively.
- Sensorineural Hearing Loss involves damage to the cochlea or vestibulocochlear (CN VIII) nerve.
- Mixed Hearing Loss may also occur, resulting from dysfunction of air and bone conduction.
- Functional (or psychogenic) hearing loss is nonorganic and unrelated to detectable structural changes in the hearing mechanisms; often, it is a manifestation of an emotional reaction.
Clinical Manifestations
Deafness is the partial or complete loss of the ability to hear. Due to its insidious nature, those the individual interact with are often the ones to notice deficiencies in hearing acuity.
- Early Manifestations: tinnitus, increasing inability to hear when in a group, the need to turn up the volume of a television.
- Changes in Attitude, Ability to Communicate, and Environmental Awareness (and therefore quality of life)
- In a classroom, a student with hearing loss may become inattentive, uninterested, and have failing grades.
- Individuals may miss parts of conversation, and lead to decreasing interaction, leading to feelings of isolation.
- Other changes include speech deterioration (volume, articulation), fatigue (straining to hear), insecurity, indecision and procrastination, suspiciousness, false pride, and tendencies to dominate the conversation (to avoid having to listen).
Prevention
Many environmental factors affect the auditory system and, with time, result in permanent sensorineural hearing loss. The most common of these is noise. Loud, persistent noise has been found to constrict peripheral blood vessels, increase blood pressure and heart rate (adrenalin), and increase gastrointestinal activity. Noise can produce a sense of unease and anxiety. Risk factors include:
- Congenital malformations of the cranial structure (ear)
- Family history of sensorineural impairment
- Low birth weight (<1500 g)
- Tympanic Membrane Perforation
- Recurrent ear infections
- Use of ototoxic medications (e.g., gentamycin, loop diuretics)
Damage from continued noise begins at a minimum of 85 to 90 dB, where permanent hearing loss from damage to the hairs of the organ of corti. Legal restrictions on occupational noise around or below that level, peaking at 135 dB.
There is no prevention known for presbycusis, the loss of hearing associated with age. Read more here.
Treatment
For conductive hearing loss, treatment of the causative factor may be effective in restoring hearing. For long-term, permanent hearing loss, for if the cause is untreatable, or for patients who do not wish to be treated, aural rehabilitation may be beneficial.
Nursing Management
Early detection is important. Ask the questions “Have you experienced any hearing loss in the past? Now?”, and “Do your family members think that you are having difficulty hearing or experiencing any hearing loss?“.
- Understanding of the types of hearing loss helps with enhancing communication with patients. The use of louder speech will only impede communication when speaking with a patient with high-frequency hearing loss. The use of other techniques, such as speaking to the better ear, and using gestures and facial expressions can help.
External Ear Disorders
Cerumen Impaction
Cerumen is a normal secretion of the cerumenous glands in the outer part of the meatus, producing ear wax. It is initially colorless and semi-liquid, but changes to pale yellow, golden yellow, to light brown, then finally black. During this change in color, the wax also hardens, and becomes denser. When enough cerumen builds up and hardens, it may block the ear canal and produce impaction, which can also cause otalgia, with or without hearing loss.
- Home Treatment: soften the wax in the ear with mineral oil, baby oil, glycerin, commercial drops, and detergent drops (e.g. 50% hydrogen peroxide, ceruminolytic agents [Carbamide peroxide] b.i.d/t.i.d). This can also be done 30 minutes before an irrigation.
- Irrigation: body-temperature water (cold water can cause vomiting), with the head upright, is instilled with a syringe (at the lowest pressure possible) against the ear canal wall next to the wax plug. Afterwards, tip the head to drain the water. Repeat several times as needed. Once the wax is removed, the ear should be dried thoroughly. Drying can be helped by a few drops of alcohol in the ear or a hair dryer set on low. Never irrigate the ear if integrity of the ear drum is questionable. This may lead to infection or acoustic trauma.
- If attempts to remove the wax plug is unsuccessful, consult a health care provider. They may repeat irrigation, suction the ear canal, or use a cerumen curette. Instrumentation may only be done by otolaryngolosits and nurses with special training due to the risk of perforating the tympanum or excoriating the thin skin of the external auditory canal.
Foreign Bodies
Any number of small objects can be lodged into the ear canal e.g. peas, beans, pebbles, toys, beads, insects, etc. Manifestations may range from no symptoms to severe pain and hearing loss. Irrigation, suctioning, and instrumentation may be attempted, same as in Cerumen Impaction. Contraindication for irrigation is the same. Vegetable-type foreign bodies may swell with irrigation, and is therefore also contraindicated. Risks of perforation and excoriation suggest that removal of foreign bodies should not be done by unskilled individuals.
Any object that has been lodged in or penetrated through the ear canal.
- Calm down and reassure the patient.
- If the object is sticking out, gently remove it by hand or with tweezers. Get medical help to ensure that no remaining foreign bodies have been left inside the ear. Do not attempt to remove remnants if not clearly visible.
- Attempt to use gravity to remove the object. Never strike the head to try and get it out. Gently shake the head in the direction of the ground to try and dislodge the object.
- If the object remains inside, seek medical help.
If the foreign body is an insect e.g. ants, mosquitos, spiders, and cockroaches:
- Do not insert a finger or objects into the ear canal. The insect may sting or bite when aggravated.
- Point the ear canal up, and wait to see if the insect flies out or craws out.
- If the insect remains, attempt to pour mineral oil, olive oil, or baby oil into the ear. Pull the ear lobe gently (back, up for adults; back, down for children) to facilitate irrigation. The insect should suffocate and float out in the oil. Oil should only be used for insects, as other objects may absorb the oil and swell.
Otitis Externa
Also known as swimmer’s ear. It is an infection of the skin lining along the ear canal. It is often caused by a dermatosis (psoriasis, eczema, seborrheic dermatitis), and even allergic reactions.
- Incidence: common in pre-school and school-age children.
- Causative agents: Staphylococcus aureus, Pseudomonas sp., or sometimes the fungus Aspergillus can enter the ear canal from a scratch, injury, or if the ear is wet for a prolonged period of time. Systemic conditions (vitamin deficiency, endocrine disorders) may also be a cause.
Clinical Manifestations
Itching, pain in the ear canal, small amounts of clear discharge, and occasionally a fever and/or hearing loss, cellulitis, and lymphadenopathy.
- Diagnostic Examination:
- The auricle and ear canal appears red and swollen. The ear canal may appear to have eczema (scaly shedding of skin).
- The outer ear is tender.
- The eardrum may be obstructed because of swelling of the outer canal.
- Growing culture from the clear discharge may identify the causative bacteria or fungus.
Treatment
The goal is to cure the infection.
- Clean the canal of drainage to allow topical medications to work effectively.
- Antimicrobial or antifungal otic medications may be used. For bacterial infections, a combination of antibiotics and corticosteroid otic drops are used to fight infection, reduce itching, and reduce inflammation. It is used abundantly (4 or 5 drops at a time) in order to reach the end of the ear canal.
- In severely obstructed ear canals, a wick may be used to facilitate the instillation of medicine.
- Analgesics may be used for severe pain for the first 2 to 4 days.
- A Warm Compress may reduce pain.
- Keep the ears clean and dry, even during showering, shampooing, or bathing. Do not swim.
Nursing Management
Prevent infection. Recurrence is highly likely unless the patient allows the external canal to heal completely.
- Inform the patient to avoid cleaning the external auditory canal with cotton-tipped applicators to avoid events that traumatize the external canal, such as scratching.
- Avoid getting the canal wet, even when bathing. A cotton ball covered in a water-insoluble gel (e.g. petrolatum jelly) can act as a barrier for the ear.
- Do not swim for 7 to 10 days after diagnosis.
- Antiseptic otic preparations after swimming can prevent infection (contraindicated in history of tympanic membrane perforation or on-going infection).
Middle Ear Disorders
Disorders affecting the incus, malleus, stapes, ear drum, and eustachian tube.
Tympanic Membrane Perforation
Perforation caused by infection (rupturing from middle ear pressure) or trauma. These include skull fractures, injury from explosion, or severe blows to the ear. Less frequently, these can be caused by Foreign Bodies that have been pushed too far into the external auditory canal. Injury to the ossicles and even the inner ear can be associated with tympanic membrane perforation.
Treatment
Most perforations heal spontaneously within weeks, or months. Some persist when scar tissue grows on the perforation, and prevents extension of the epithelial cells across the margins and final healing.
- In cases of head injury or temporal bone fracture, a patient is observed for CSF otorrhea or rhinorrhea.
- While healing, protect the ear from water entering the ear canal.
Surgical management (Tympanoplasty) can be done for prevention of infection or to restore hearing. It is performed on an outpatient bases and can be done with various techniques; grafting (usually from temporalis fascia) can allow healing and closing the perforation permanently, and improving hearing.
Otitis Media
An inflammation and/or infection of the middle ear. This may manifest as acute or chronic otitis media. Both may be suppurant or purulent otisis media. Inflammation of mucosa occurs, then swelling and irritation of ossicles, then purulent inflammatory exudate is produced.
Clinical Manifestations
- Acute Otitis Media (AOM) lasts for less than 6 weeks, caused by bacteria or viruses. Two common portals of infection is through the eustachian tube (obstruction related to URTI, inflammation of surrounding structures, or allergic reactions), or through a perforated tympanic membrane. A purulent exudate is often present in the middle ear, producing conductive hearing loss.
- Clinical Manifestations: often unilateral. Accompanied by otalgia. Pain is relieved after spontaneous perforation or a tympanectomy. Drainage, fever, and hearing loss may also be present. Sleep may become disturbed.
- In infants, irritability and inconsolable crying (clearest sign) can point to AOM.
- Risk Factors: younger age (shorter ear canal and eustachian tube), chronic URTIs, chronic exposure to secondhand cigarette smoke.
- Clinical Manifestations: often unilateral. Accompanied by otalgia. Pain is relieved after spontaneous perforation or a tympanectomy. Drainage, fever, and hearing loss may also be present. Sleep may become disturbed.
- Chronic Otitis Media: a recurrent form of AOM that causes irreversible tissue pathology. These damage the tympanic membrane, destroy the ossicles, and involve the mastoid, but are rarely found in developed countries.
- Clinical Manifestations: symptoms may be minimal, with varying degrees of hearing loss and a persistent or intermittent, foul-smelling otorrhea. Pain is not usually experienced, except in cases of acute mastoiditis, when the postauricular area is tender and may be erythematous and edematous. Otoscopic examination may show a perforation, and a cholesteatoma can be identified as a white mass behind the tympanic membrane or through to the external canal from a perforation.
- Chronic mastoiditis can result in cholesteatoma formation, a cystlike lesion in the middle ear, filled with degenerated skin and sebaceous materials pulled in by persistent high negative pressure. It may damage the facial nerve, horizontal canal, and other surrounding structures. They produce no pain, but can enlarge to the point where they burst or destroy the mastoid bone. In older adult patients, they generally develop in the external canal. They may cause hearing loss, facial pain and paralysis, tinnitus, or vertigo. Diagnosis is made visually, with CT, or MRI. Audiometry reveals conductive or mixed hearing loss. Treatment is surgical removal of mass after treatment of the acute infection.
- Clinical Manifestations: symptoms may be minimal, with varying degrees of hearing loss and a persistent or intermittent, foul-smelling otorrhea. Pain is not usually experienced, except in cases of acute mastoiditis, when the postauricular area is tender and may be erythematous and edematous. Otoscopic examination may show a perforation, and a cholesteatoma can be identified as a white mass behind the tympanic membrane or through to the external canal from a perforation.
- Serous Otitis Media: a middle ear effusion without the presence of an active infection. Theoretically, fluid is pulled into the cavity by negative pressure produced by obstruction of the eustachian tube. This is often seen in patients after radiation therapy or barotrauma (sudden pressure changes). A carcinoma may also block the tube and should be suspected in patients with persistent unilateral serous otitis media.
- Clinical Manifestations: fullness in the ear, sensation of congestion, popping or crackling noises (when the eustachian tube attempts to open), hearing loss.
- The tympanum appears dull upon otoscopy. Air bubbles may be visualized. Usually, audiogram shows conductive hearing loss.
- Management: no treatment unless AOM occurs. A drainage tube myringotomy can be performed if severe. Barotrauma-induced edema of the eustachian tube can be relieved by corticosteroids. A Valsalva procedure can open the eustachian tube, but also carries the risk of worsening pain or rupturing the tympanum.
Diagnostic Examination
Otoscopy reveals an opaque, bulging/retracted tympany
- Erythema of the tympanic membrane
- Accumulation of fluid (potentially blood or purulent) behind the eardrum.
- Signs of perforation should be checked.
- Check for signs of drainage.
- Perform audiometry for patients with long-standing otitis media.
Medical Management
The goals of treatment is treating the infection and minimizing symptoms:
- Relieve Pain: analgesics, avoid chewing during acute period, lie with affected ear down; Relieve Fever: antipyretics
- Curing the Infection: antibiotics
- Preventing Complications: screening for hearing loss may be necessary.
- Preventing recurrent ear infections
Surgical Management
If condition persists with antibiotic treatment, and fluid remains in the middle ear, a Myringotomy or Tympanectomy relieves pressure and allows drainage of the fluid. A small incision is made in the eardrum, and the accumulated fluid is suctioned. The incision does not require suturing, and seals itself spontaneously. A drainage tube may be inserted to dry out the middle ear and prevent the fluid from re-accumulating. They fall out after a few months, but can also be removed in the doctor’s office if they remain.
- Type I Tympanoplasty: Myringoplasty, designed to close a perforation in the tympanic membrane.
- Types II to V extensively repair the middle ear structures. These all work to restore the sound conduction mechanisms.
- Moderate sedation or general anesthesia is used, and these surgeries are mostly outpatient-based. Patients often recover significantly upon closure of a perforation or reestablishment of the ossicles.
- Ossiculoplasty: reconstruction of the middle ear bones to restore hearing. Prosthesis such as Teflon, stainless steel, and hydroxyapatite are used to reconnect the ossicles.
- Mastoidectomy: done for removal of cholesteatomas; gain access to diseased structures; and create a dry, noninfected and healthy ear. If possible, ossicles are reconstructed during this procedure. Extensive damage may split this procedure into a two-stage operation; checking for recurrent or residual cholesteatoma. Success rate is 75% for correcting conductive hearing loss.
- A pressure dressing is applied and kept for 24 to 48 hours after the procedure.
- Report and facial paresis to the primary provider, as the facial nerve may rarely be damaged from a mastoidectomy.
Versus Acute Otitis Externa
| Difference | Acute OE | Acute OM |
|---|---|---|
| Ear Canal | Swollen | Normal |
| Tympanum | Normal (or red) | Red, bulging, potentially perforated |
| Otorrhea | Maybe | Yes, through perforation |
| Otalgia | Persistent | Relieved once ruptured |
| Aural/Tragus Tenderness | Yes | No |
| Edema of Ear Canal | Yes | No |
| Fever | Yes | Yes |
| Systemic Symptoms | None | Fever, URTI, Rhinitis |
| Hearing | Normal or Decreased (Conductive) | Decreased (Conductive) |
| Season | Summer | Winter |
Mastoiditis
Infection of the mastoid bone of the skull, often as a consequence of Otitis Media. The infection may spread from the ear to the mastoid bone, and the mastoid bone fills with infected materials, and its honeycomb-like structure may deteriorate.
- Clinical Manifestations
- Ear pain or discomfort
- Otalgia
- Pain behind the ear
- Redness of the ear or behind the ear
- Fever (high or spiked)
- Headache
- Otorrhea
- Diagnostic Examination
- Imaging: A skull x-ray or head/ear CT scan may show abnormalities of the mastoid bone.
- Culture of drainage from the ear may show bacteria.
- Treatment
- Medications have difficulty penetrating into the mastoid bone. It may require repeated or long-term treatment. Parenteral then oral antibiotics are given for the infection.
- Surgery may be required if antibiotic therapy is not successful.
- Mastoidectomy: removing part of the bone and draining the mastoid of infected materials.
- Myringotomy: for underlying middle ear infection.
- Tympanoplasty: repairing or reconstructing the tympanum to help restore normal hearing.
- Ossiculoplasty: repairing or reconstructing the ossicles.
- Post-op: monitor for dizziness, meningitis, edema, drainage, and redness.
- Wound dressing change 24 hours post-op.
- Position patient flat with operative side up.
- Assist the patient in rising and ambulation.
Otosclerosis
The stapes/stirrup bone accumulates extraneous bone formation (callus) and creates a partial fixation, limiting movement of the stapes and resulting in conductive hearing loss. This may result in complete deafness.
- The cause is unknown. About 50% of patients have a family history. Some studies show measles virus as a factor, and that pregnancy can accelerate formation of bone callus (female sex hormones worsen otosclerosis)
Clinical Manifestations
The primary symptom of otosclerosis is slowly progressing conductive hearing loss beginning anytime between the age of 15 and 45, usually around 20.
- Patients may state that they hear better in noisy surroundings, as the raised frequency and intensity of sound allow the stapes to move properly.
- Constant Tinnitus may be present.
- The tympanic membrane is normal.
- Balance problems: unsteadiness, dizziness, vertigo, other senses of motion.
- Schwartze’s Sign: a pink-blush hue behind the tympanic membrane
- Negative Rinne’s Test
- Lateralized Weber Test
- Bilateral Hearing Loss
Treatment
There is no known cure for otosclerosis.
- Oral fluoride supplementation is a disease-modifying therapy, nearly halting disease progression.
- Dizziness associated with active otosclerosis often respond within two weeks of oral fluoride therapy.
- Stapedectomy: the ear drum is turned forward and the fixed stapes is removed. A stapes prosthesis (teflon or metal) is inserted and attached to the anvil, then the ear canal is filled with ointment. This results in (usually) permanent hearing. Hearing aids should be considered if hearing is still insufficient.
- Stapedotomy: a hole is placed in the oval window and a prosthesis is inserted, but the stapes is not removed.
Inner Ear Disorders
Meniere’s Syndrome (Endolymphatic Hydrops)
A disorder of the inner ear affecting balance and hearing. The inner ear has a series of canals, which separate important fluids (endolymph, perilymph) and prevent them from mixing. When they mix (like if a rupture between the canals was present), the microscopic hair cells (a major component in hearing and balance) stiffen, become bent, or broken.
- Etiology: swelling of part of the canal (endolymphatic sac). Exact cause is unknown. It may be related to Otitis Media, syphilis, head injury, recent viral illness, respiratory infection, stress, fatigue, use of drugs, allergies, smoking, alcohol use, and genetic risk factors.
Clinical Manifestations
- Episodes of vertigo (may be episodic; minutes to 8 hours, worse with sudden movements) or dizziness.
- Fluctuating, progressive, low-frequency hearing loss in one ear.
- Tinnitus
- Nausea and Vomiting
- Sweating (may be profuse)
- Uncontrollable eye movements (Nystagmus; compromised vestibulo-ocular reflex?)
- Sensations of fullness or pressure in the ear.
Diagnostic Examination
A neurologic examination may show abnormalities of cranial nerve VIII (vestibulocochlear), such as abnormalities of hearing, balance, or eye movement. Tests to distinguish Meniere’s disease from other causes of vertigo may include:
- Head CT Scan or MRI
- BAER
- ENG with Caloric Stimulation Test (abnormal results indicate Meniere’s disease)
- Audiometry to check for the extent of hearing loss.
Treatment
There is no known cure for Meniere’s disease. Treatment is focused on lowering the pressure within the endolymphatic sac and symptomatic treatment, which tend to occur in discrete attacks.
- Antihistamines, Anticholinergics, and Diuretics may lower the amount of endolymphatic fluid, and therefore pressure.
- A low-salt diet reduces fluid retention.
- Symptoms such as dizziness, vertigo, and associated N&V may respond to sedative/hypnotics, benzodiazepines like Diazepam, and anti-emetics.
- Labyrinthectomy, Endolymphatic Sac Surgery, or Vestibular Nerve Surgery may be required if symptoms are severe and are unresponsive.
- Hearing Aids may be needed for severe hearing loss.
- Avoid sudden movements that may aggravate symptoms.
- Ambulatory aid may be required.
- Rest during severe episodes, and gradually increase activity.
- Avoid bright lights, TV, and reading during attacks, which may make symptoms worse.
- Avoid hazardous activities until one week after symptoms disappear.
Presbycusis
A sensorineural hearing loss that occurs as a result of aging. This occurs in 25% of people aged 65 to 75, and in 70 to 80% of those over age 75. Other changes include harder and drier cerumen, sclerotic or atrophied tympanum, and cochlea degeneration. Higher frequency hearing loss appears first, followed by middle and lower frequencies.
- Causes: degeneration or atrophy of the ganglion cells in the cochlea, loss of elasticity of the basilar membrane, decreased blood supply to the inner ear, vitamin B9 and B12 deficiencies, atherosclerosis, hypertension, infections, prolonged fever, Meniere’s disease, DM, ear surgery, and trauma to the ear or head. It may also be psychogenic. Ototoxic drugs may also contribute. There appears to be a genetic predisposition.
- Clinical Manifestations: loss of hearing occuring slowly over time. This often starts with high-frequency sounds. Noisy areas may make it difficult to listen to any particular sound. The patient often also develops depression, isolation, and a decrease in cognitive function. Feelings of isolation, confusion, alterations in ADLs, and increasing risk of falls are all associated with hearing loss.
- Diagnostic Examination: wax in the ear can contribute to hearing loss. Audiometry determines the extent of hearing loss.
- Treatment: no known cure; focused on functional improvement. Hearing aids may help. Lip-reading and using visual cues may also aid in communication, but may be hard to learn for older people.
Otic Medication Administration
- Wash hands. Maintain hygiene to prevent contamination of medication and the ear.
- Warm and shake the bottle of medication.
- Lie on the side with the infected ear facing up.
- Obtain 3 to 5 drops (as instructed) put into the infected ear. Do not touch the bottle onto any surface.
- For patients with otitis media, press the tragus (gently) five times in a pumping motion to allow the drops to pass through the tube. For patients with otitis externa, pull the earlobe backwards and upwards (adults) or backwards and downards (children) to straighten the ear canal and facilitate administration.
- Remain on the side for at least 60 seconds. Repeat for the other side if it is also infected.