The Nursing Process is used in the delivery of nursing care service. It follows the ADPIE format: Assessment, Diagnosis, Planning, Intervention, Evaluation.
Patient Classification System
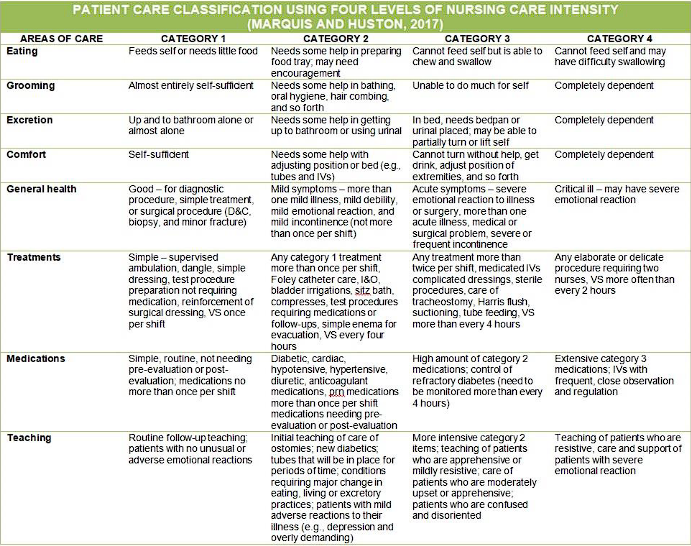
As the name suggests, a PCS (A.K.A. Workload Management, Patient Acuity Tools) groups patients according to their acuity of illness and the complexity of necessitated nursing activities. The totality of projected nursing needs for the succeeding shifts is typically based on patient acuity data, collected every shift. Using the PCS provides an objective approach to determine staffing based on patient care needs. Basically, the more sick people, the more nurses required.
Barriers
Barriers to the use of PCS include the lack of standardization, a lack of credibility, and a lack of consideration for patient flow (Hertel, 2012).
| PCS Acuity or Level of Care | Nursing Care Hours Required |
|---|---|
| Level 1: Self-Care or Minimal Care | 1.5 |
| Level 2: Moderate or Intermediate Care | 3.0 |
| Level 3: Total or Intensive Care | 4.5 |
| Level 4: Highly Specialized or Critical Care | 6.0 or 7.0 hours or more |
- Level 1: patients who are recovering, often requiring only diagnostic studies, minimal therapy, less frequent observations, and daily care for minor conditions and are awaiting elective surgery.
- Level 2: moderately ill or recovering from serious illness or an operation. They require nursing supervision or assistance that is related to ambulating and caring for their own hygiene.
- Level 3: patients need close attention and complete care all throughout the shift. The nurses initiate, supervise, and perform most of the patient’s activities.
- Level 4: acutely ill patients with a high level of nurse dependency
Patient classification systems are institution-specific and must be modified to reflect the unique staff and patient population of each organization. Maybe other variables also make it difficult to simply transfer a PCS from one facility to another. Here’s one example (too much info that I don’t think will be relevant given the preceding statement):
Modalities of Care
Caregiving in an organization will naturally require some method of labor division and assignment. In the field of nursing, there are five well-known methods for organizing patient care:
| Method | Basic Principle |
|---|---|
| Case Method Nursing | ”Total Patient Care”. The oldest; patients are assigned as cases to nurses, who take total responsibility for their needs. |
| Functional Nursing | Task-based assignment based on nurse competence and specialty. |
| Team Nursing | A professional nurse coordinates ancillary personnel to provide care to a group of patients. |
| Modular Nursing | A refined form of team nursing, forming smaller teams or even pairs of at least one registered nurse. |
| Primary Nursing | ”Relationship-based nursing”. A primary nurse assumes responsibility for planning the care patient/s from admission to discharge. |
| Case Management | Highly individualized care created from a collaborative process of assessment, planning, facilitation, and advocacy by case managers. |
| Case Method Nursing or Total Patient Care Nursing is the oldest mode of organizing patient care. Nurses assume total responsibility during their time on duty for meeting all needs for assigned patients. Planning is less necessary, and the lines of responsibility and accountability are clear. |
- Pros: the nurses receive high autonomy and responsibility, allowing for holistic and unfragmented care during the nurse’s shift.
- Cons: care may become fragmented between shifts, there is less efficiency as the specialized nurse performs tasks that could be delegated instead, and most importantly, the necessitated competency on nurses to handle autonomy— inexperienced nurses may fail to provide total care for the patient.
Functional Nursing evolved from the great shortage of nurses after the second world war. Relatively untrained workers were trained to perform simple tasks and gained proficiency by repetition. Personnel are assigned to tasks rather than patients, e.g., a nursing aide handles all vital signs monitoring, one registered nurse handles all the medications required, etc.
- Pros: high efficiency in times of high demand, accommodating for many levels of competency. Nurses become managers of care rather than direct providers.
- Cons: care is fragmented, and patient needs may be overlooked. Job satisfaction may also be low. The need for many care coordinators may increase costs.
Team Nursing handles a group of patients under the supervision of a professional nurse (often chosen democratically) who shares responsibility in care. The team leader must know the condition and needs of all the patients for planning individual care. The role of the team leader can vary, from coordinating patient activities to giving direct personal care to patients.
- Cons: an extensive amount of communication is required, and teams are limited to ≤5 people, as large teams will revert to functional lines of organization. The team leader requires excellent communication and organizational/leadership skills to properly implement this type of care.
Modular Nursing is a refined form of team nursing, as team nursing was mostly never practiced in its purest form. Modular nursing changes this by forming smaller teams (mini-teams, care pairs— 2 or 3 people) with at least one registered nurse. These teams are often assigned geographically.
- Pros: a smaller team requires less coordination and communication, allowing more time for direct patient care activities.
Primary Nursing, also known as relationship-based nursing, was developed in the late 1960s. It takes from Total Patient Care and involves bedside care: the primary nurse assumes 24-hour responsibility for planning the care of assigned patients from admission to discharge. This care is provided directly by the primary nurse during their shift, and followed by associate nurses otherwise.
- Pros: clear interdisciplinary group communication and consistent, direct patient care by relatively few nursing staff allows for holistic, high-quality patient care. Additionally, this type of nursing can be applied in other contexts, e.g., hospice care, home nursing. Job satisfaction is also high, as nurses feel challenged and rewarded.
- Cons: improper implementation fails to coordinate a multidisciplinary team or fails to identify complex patient needs and changes in condition. High experience and skills are necessary for this role.
Case Management is a collaborative process of assessment, planning, facilitation, and advocacy for options and services to meet an individual’s health needs through communication and available resources to promote quality cost-effective outcomes. This process, handled by the case manager, often uses critical pathways and multidisciplinary action plans (MAPs) to plan patient care; the Care MAP is a combination of a critical pathway and a nursing care plan.
- Pros: each patient is considered individually to identify the most cost-effective care setting possible. Community resources, providing healthcare information, and testing and procedures are all included in care.
- Cons: being a case manager requires extensive knowledge and experience. This role is argued to be reserved for advance practice nurses or those with advanced training.
Contemporary Models of Care
| Model | Basic Principle |
|---|---|
| Professional Nursing Practice Model | A framework for guiding and aligning clinical practice, education, administration, and research in order to achieve positive patient and nurse staff outcomes. This is a core feature of magnet hospitals. |
| Differentiated Nursing Practice Model | The provision of care is differentiated according to the level of competency of the RN, scaling responsibility with expertise. |
| Clinical Nurse Leader Model | A clinical nurse leader (CNL) designs, implements, and evaluates patient care by coordinating an interprofessional team in the provision of care. They are a provider and coordinator of care (rather than a manager and leader) and fosters inter- and intraprofessional communication. |
| Synergy Model for Patient Care | ”Synergy” occurs when the needs and characteristics of the patient, clinical unit, and/or system are matched with the nurse’s competencies. |
| Transforming Care at the Bedside | The main goal of this model is to improve patient care and decrease turnover (improve employee retention). It involves five themes: transformational leadership, safe and reliable care, vitality and teamwork, patient-centered care, and value-added care processes. |
| Patient-Centered and Family-Centered Care Model | This model emphasizes the inclusion of patients and their families in collaboration, no matter their age, level of care, and healthcare setting. The patient retains control over their care, and all healthcare decisions are made with the RN as a collaborator. |
Organizational Structure
Fayol postulates that an organization is created once the number of workers begins to necessitate a supervisor. Organizations allow for collective effort, outweighing individual effort.
Venzon (2016) on Organizations
“It pertains to the body of persons, methods, policies and procedures arranged in a systematic process through the delegation of functions and responsibilities for the accomplishment of purpose.”
Organizational structure is divided between formal and informal structure. In formal structure, managerial authority, responsibility, and accountability is clearly defined; roles and functions are outlines, people have specific tasks to perform, and rank and hierarchy are apparent.
On the other hand, informal structure is the channel that “fills in the gaps with connections and relationships that illustrate how employees network with one another to get the work done.” As supported by Schatz (2013) informal structures are typically centered on camaraderie and often produce direct response from individuals, saving time and effort. It is also useful when the formal structure becomes non-effective.
The communication network used for informal structure is grapevine, consisting of exchanges in the break room, in the hall way, in a carpool, in between work, and online that allows relationships of informal groups to develop.
Organizational Theory and Bureaucracy
Revisiting Max Weber, he states that bureaucracy is an institutional method for applying general rules to specific cases, making the actions of management fair and predictable. Other characteristics of bureaucracy include:
- A clear division of labor.
- A well-defined hierarchy of authority, separating superiors from subordinates. There must be remuneration for work, recognition of authority, allotment of privileges and conferring of promotions.
- There must be impersonal rules and impersonality of interpersonal relationships.
- A system of procedures for dealing with work situations must exist.
- A system of rules covering the rights and duties of each position must be in place.
- Selection for employment and promotion is based on technical competence.
To highlight the structure and order of an organization, an organizational chart utilizes a line drawing that diagrammatically shows the formal organizational relationships, areas of responsibility, superiors of subordinates, and channels or organization. In filling out an organizational chart, organizing must take place. It involves the establishment of formal authority and producing structure by identifying groupings, roles, relationships, and staffing patterns. Each role involves job descriptions, qualifications, and functions.