Reference
Salustiano, R. (2024). The Fetus During Labor. In Dr. RPS Maternal & Newborn Care: A Comprehensive Review Guide and Source Book for Teaching and Learning (2nd ed., pp. 262-270). C&E Publishing, Inc.
Column
clean
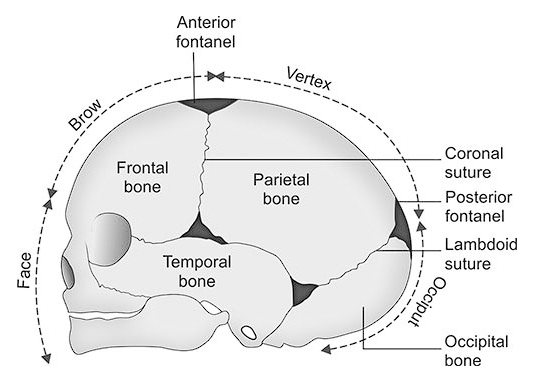
Fetal Head
The fetal head has seven bones. Two frontal, two parietal, two temporal, and one occipital. Along the adjacent edges of these bones are sutures, and the meeting points of multiple skull bones are fontanels.
- Sagittal Suture: longitudinal, midline
- Frontal Suture: anterior suture between two frontal bones.
- Coronal Suture: anterior suture between frontal and parietal bones.
- Lambdoidal Suture: posterior suture between parietal and occipital bones.
INFOBOX
Fetal Skull
- Anterior Fontanel: formed by two frontal bones and two parietal bones. It is diamond-shaped, measures 2.5 cm × 2.5 cm, and ossifies in 12 to 18 months.
- Posterior Fontanel (Lambda): formed by the union of two parietal bones and one occipital bone. It is triangular and ossifies in 6 to 8 weeks or 2 to 3 months.
| Fetal Skull Diameters | ||
|---|---|---|
| Anteroposterior Diameters | Width | Description |
| Occipitomental | 12.5-13.5 cm | Widest; from the occiput to the chin. |
| Occipitofrontal | 12 cm | From the occiput to midfrontal bone |
| Suboccipitobregmatic | 9.5 cm | Narrowest; from below the occiput to the anterior fontanel. |
| Transverse Diameters | ||
| Biparietal | 9.5 cm | Widest; distance across the two parietal bones. |
| Bitemporal | 8 cm | Distance across the two temporal bones. |
| Bimastoid | 7 cm | Distance between the two mastoid processes. |
Fetal Lie
The relationship of the long axis of the fetus to the long axis of the mother’s uterus/spine.
- Longitudinal: the fetal and maternal axes are parallel. This can be further classified as cephalic or breech presentation depending on which part enters the pelvis first.
- Transverse Lie: the long axis of the fetus is perpendicular to the mother’s spine; shoulders present.
Fetal Attitude
The relationship of the fetal parts to the trunk or to one another.
- Flexion: the desired attitude.
- Extension
Fetal Presentation
The lowermost part in the pelvic inlet; the part felt upon internal examination.
- Cephalic: the head is the presenting part.
- Vertex: head acutely flexed
- Sinciput: head moderately flexed
- Brow: head moderately extended
- Face: head acutely extended
- Breech: the buttocks are the presenting part. FHT is felt at the upper quadrants or above the level of the umbilicus, and with the findings of Leopold’s maneuvers 1 (hard, round, ballottable mass) and 3 (soft, globular, non-ballottable mass).
- Complete (Full): feet and legs are flexed on the thighs; buttocks and feet presenting; fetus squatting; the type favoring most the second stage of labor as the feet could be used as traction.
- Incomplete (Frank): thighs flexed against the abdomen; legs extending up to the shoulders as they lie on the anterior chest; buttocks present; the type favoring most the first stage of labor as the large buttocks are a good dilating wedge.
- Footling (single or double): one foot or two present; the type is easily complicated by cord prolapse.
Meconium Staining
If the fetus is breeched, the passage of meconium staining is not a sign of fetal distress.
- Shoulders: usually referred to as a transverse lie; the fetal long axis lies perpendicular to the maternal spine, and the fetus appears to lie crosswise in the uterus.
Fetal Position
Position refers to the relationship of the denominator or landmark of the presenting part to the front imaginary quadrants of the mother’s pelvis. Assessment of the position can be done through Leopold’s maneuvers, vaginal examination, and rectal examination (obsolete).
- Chosen Landmarks/Denominators:
- Occiput (O) for vertex presentation
- Mentum (M) for face presentation
- Sacrum (S) for breech presentation
- Acromiodorso (AD) for shoulder presentation
- Four Imaginary Quadrants:
- Left anterior
- Right anterior
- Left posterior
- Right posterior
| Occiput | Mentum | Sacrum | Acromiosdorso | |
|---|---|---|---|---|
| Left Anterior | LOA | LMA | LSA | LAPA |
| Right Anterior | ROA | RMA | RSA | RAPA |
| Left Posterior | LOP | LMP | LSP | LAPP |
| Right Posterior | ROP | RMP | RSP | RAPP |
- Left occipitoanterior (LOA) features the occiput pointing towards the mother’s left abdominal wall, face is down towards the maternal right buttocks; most common and favorable position.
- Occiputposterior (OP), either left (LOP) or right (ROP), is a factor in prolonged labor, with the mother experiencing much discomfort (backache) during labor. Comfort measures: side-lying, backrub, counter-sacral pressure during contractions.
Column
Note
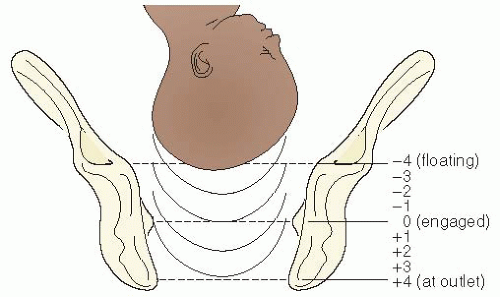
Fetal Station
Station refers to the relationship of the presenting part to the ischial spines, the single most important landmark of the pelvis. It measures how far the presenting part has descended into the pelvis— the degree of descent. Each station is one centimeter and determined through internal examination.
- Floating (High; Ballottable): unengaged presenting part
- Station 0: the presenting part is at the level of the ischial spines.
- Minus Station (Negative): if the presenting part is above the level of the ischial spines, station is expressed as a negative number (e.g., -1 (1 cm above), -2 (2 cm above)).
- Plus Station (Positive): if the presenting part is below the ischial spines (outlet), station is expressed as a positive number (e.g., +1 (1 cm below), +2 (2 cm below)).
Infobox
Stations
Score Meaning -5 to 0 The “presenting” or most palpable (able to feel) part of the baby is above the woman’s ischial spines. 0 The baby’s head is known to be “engaged,” or aligned with the ischial spines. 0 to +5 Positive numbers are used when a baby has descended beyond the ischial spines. During birth, a baby is at the +4 to +5 station.
Fetal Well-Being in Labor
Fetal well-being can be determined by fetal heart rate/tone, fetal movement (at least three per hour), and the presence of meconium in non-breech presentations (a sign of fetal distress).
Fetal Heart Tone
The fetal heart rate is the best measure of fetal well-being. There are several parameters related to FHR:
- Baseline Fetal Heart Rate: FHR between contractions and accelerations. To get the baseline FHR, get two FHR strips of at least 10 minutes each and compare.
- Fetal Heart Rate Variability: fluctuations in the FHR, either long-term or short-term.
- Long-Term Variability (LTV) are slow, rhythmic fluctuations above and below the average baseline rate, producing a wavelike pattern. The criteria for LTV do not include acceleration or decelerations. Findings for LTV may be:
- Reassuring: two spontaneous accelerations of greater than 15 BPM for at least 15 seconds’ duration in 20 minutes.
- LTV Absent: a “flat” FHR; some causes may be CNS depressants from the mother, hypoxia due to placental insufficiency, severe fetal anemia, or fetal brain anomaly/death.
- LTV Chaotic: jumping up and down multiple times per minute; marked LTV or saltatory pattern. When LTV is present, STV is almost always present.
- Short-Term Variability (STV): is beat-to-beat variability, which is instantaneous fluctuations in FHR. The combination of long-term and short-term variability reflects the interaction between the sympathetic (which accelerates the heart rate) and parasympathetic (which slows the heart rate) branches of the central nervous system (CNS); it indicates an intact fetal central nervous system. For STV to be visualized, it needs internal FHR monitoring. It can be present in the absence of LTV.
- Long-Term Variability (LTV) are slow, rhythmic fluctuations above and below the average baseline rate, producing a wavelike pattern. The criteria for LTV do not include acceleration or decelerations. Findings for LTV may be:
- Periodic Fetal Heart Rate Changes are transient changes in FHR in association with contractions.
- Nonperiodic Fetal Heart Rate Changes are transient changes in FHR not associated with contractions, although they can occur during contractions:
- Acceleration: an increase in FHR above the baseline level, with a return to baseline within 10 minutes. An increase in FHR lasting longer than 10 minutes is classified as an increase in FHR baseline. Accelerations are the most common type of FHR change.
- Deceleration: a distinct decrease below the baseline, with a return to the baseline within 10 minutes. Decelerations are classified by their shape and timing in relation to uterine contractions:
- Early Deceleration (U-shape): decrease, but not below 100 BPM. It occurs early, before acme, and is characterized by a gradual onset at the beginning of a contraction and a slow return to the baseline soon after the contraction ends. This indicates fetal head compression in early contractions and as it enters the birth canal, which stimulates the vagus nerve to decrease FHR. Normally benign; no need for nursing intervention.
- Variable Deceleration (V- or W-shape): occurs at any point. It is believed to be caused mostly by cord compression, featuring abrupt swings in FHT and a rapid return to baseline. It is most frequently observed after rupture of membranes, when there is less amniotic fluid to provide a protective cushion around the cord. While usually not an ominous sign, it requires continuous nursing assessment. The nurse may change maternal positioning to relieve cord compression. If no improvement occurs, administer oxygen, stop oxytocin if infusing, and prepare for an internal examination to identify cord prolapse.
- Late Deceleration: usually gradual at onset; the nadir (lowest point) of the deceleration usually occurs after the peak of the contraction; FHR decreases rarely below 100 BPM, but the FHR does not return to baseline by the end of contraction. It is caused by uteroplacental insufficiency, compromising blood flow from the placenta to the fetus; fetal distress. This is an abnormal and ominous sign.
| Deceleration | Features | Cause | Action |
|---|---|---|---|
| Early | Before acme; gradual, U-shaped | Fetal Head Compression | Benign; no action required. |
| Variable | Any point; abrupt, V- or W-shaped | Cord Compression | Continuous monitoring; positional adjustment. If improvement is not observed, administer oxygen, stop oxytocin, and prepare for an internal examination for cord prolapse. |
| Late | After acme; gradual | Uteroplacental Insufficiency | Abnormal/Ominous; discontinue oxytocin, position the mother on LLR, give oxygen (8 to 10 L/min), increase hydration, run IV (plain) faster, and prepare for delivery as indicated. |
Legal Tip
The Philippine Nursing Act of 2002 includes the care given by nurses to women in labor. It shall be the duty of the nurse to provide nursing care through the utilization of the nursing process. Nursing care includes therapeutic use of self, executing healthcare techniques and procedures, essential primary health care, comfort measures, health teachings, and the administration of written prescriptions for treatment, therapies, oral, topical, and parenteral medications; internal examination during labor in the absence of antenatal bleeding; and delivery (R.A. No. 9173).
FHR Detection
FHR is detected via auscultation. During early labor, FHR is auscultated via stethoscope every 30 minutes, and every 5 minutes in the transition phase (8 cm onwards). Counting is done for one full minute.
An electric monitor may be used as determined by hospital policy or the doctor. There are two types of FHR monitoring:
- External or Indirect Monitoring, used with intact membranes.
- Tocodynamometer: disk over the fundus, secured with a belt.
- Ultrasonic transducer: at the site of the loudest FHR, it is secured with a belt; with conducting gel over the transducer.
- Internal or Direct Monitoring, used with ruptured membranes, in the latent phase.
- Pressure transducer, an intrauterine catheter with water is inserted beyond the presenting part.
- Internal spiral electrode applied to the fetal scalp.
Factors Affecting FHR Audibility
Auscultation for the FHR can be affected by obesity, polyhydramnios, faulty equipment, environmental noise, and bowel sounds from the mother.
Point of Maximal Impulse
The point of maximal impulse (PMI) is the site where FHR is most audible. It is usually below the umbilicus along the side of the fetal back. For example,
- LOA or LOP: the fetal back is in the lower quadrants (cephalic presentation), with the occiput (hence back) facing left. The FHR can be heard best at the left lower quadrant of the maternal abdomen.
- ROA or ROP: the fetal back is also in the lower quadrants, with the back facing right. The FHR can be heard best at the right lower quadrant of the maternal abdomen.
If the fetus is cephalic but presenting with the FACE, the fetal back is difficult to palpate; a deep furrow can be palpated between the hard occiput and the fetal back as the head is acutely extended and covers the area of the fetal back. In this case, the FHR can be heard on the side where the fetal feet are palpated.
If the fetus is breech, the PMI is usually above the umbilicus and along the side of the sacrum, which is in line with the fetal back, e.g., the PMI is found in the left upper quadrant for LSA or LSP, and the right upper quadrant for RSA or RSP.
Findings
Normally, FHTs sound like a ticking clock. Other sounds include maternal soufflé and fetal soufflé.
- Maternal soufflé: also known as uterine bruit. It is the sound produced as blood moves through the uterine vessels and is synchronous with the maternal pulse; maternal in origin; does not guarantee fetal life. To determine if the FHT is not maternal soufflé, both FHT and maternal pulse is counted simultaneously. If these sounds are synchronous, it may signify fetal death. It is an ominous sign.
- Fetal soufflé: a “purring” sound heard over the pregnant uterus and having the same rate as the fetal heart beat or synchronous with FHR. This guarantees fetal life. It is fetal in origin, and is produced as blood flows/hisses through vessels in the umbilical cord.
Bradycardia is a fetal heart rate of less than 120 beats per minute (mild) or less than 100 beats per minute (severe). It may be caused by maternal hypotension, hypothermia, hypoglycemia, drugs (e.g., beta blockers), late fetal hypoxia, congenital cardiac anomalies, fetal heart failure, prolonged umbilical cord compression, and poly- or oligohydramnios. Oxygen may be administered.
Tachycardia is a fetal heart rate of more than 160 beats per minute (mild) or more than 180 beats per minute (severe). It may be caused by maternal fever, dehydration or anxiety, amnionitis, anemia, drugs (e.g., anticholinergic medications, sympathomimetic medications), early fetal hypoxia, fetal movement, neurologic immaturity, and dehydration. Oxygen may be administered.