The following notes were used for this compilation:
- Introduction to Nursing Leadership and Management
- Patient Health Care Delivery Systems
- Evidence-Based Practices in Nursing Management
- Ethical, Legal, and Moral Considerations in Nursing Leadership Management
- Organizational Communication
The pointers to review provided by Ma’am Diosul are as follows (unaltered). Basically, all the content discussed is included to some degree.
CU1
- Theories, theorists, principles
- Leadership styles
- Powers, Roles, Skills of a Manager
CU2
- Patient Classifications/Levels of Care/PCS
- Modalities of Care
CU3
- NNCCS
- Patient Safety standards
- Sentinel, Near Miss
CU4
- Code of Ethics, Related Ethical Principles
- Documentation/Patient's Records, Consent
- Contract, Will
- Criminal/Civil Case
- Doctrines
CU5
- Models of Communication
- Memos, Meeting Minutes
- External/Internal Customer Satisfaction
- Change of shift report
- Nursing Rounds
- Patient Transfer to Another Ward/To another hospitalIntroduction to Nursing Leadership and Management
Management is a universal process used in business, the practice of one’s profession, and even day-to-day personal affairs. It coordinates and supervises personnel (or the self) and available resources effectively and efficiently to accomplish organizational goals. Leadership (arguably a function of management) is the use of the self as an influencer (Leader) of a group to function together to achieve common goals and objectives.
Nursing Management
Management is an old French term meaning “the directing”. Along with the aforementioned definition, it is also used to design and maintain an internal environment in which people work together in groups that can perform effectively and efficiently towards the attainment of group goals. It may be used in running a business, in practicing one’s profession, and even day-to-day interactions.
Venson (2010)
Management is a process by which a cooperative group directs actions towards common goals, involving techniques with which a distinguished group of people coordinates the services of people. It also includes moral and ethical standards in the selection of right ends towards which managers should strive.
Harbinzon and Myers created a Three-Fold Concept to Emphasize the Broader Scope of Management:
- Economic Source: one of the factors of production, together with land, and capital. Industrialization increases, management is substituted by labor and capital. Management of a firm determines, to a large extent, its productivity and profitability.
- System of Authority: management first develops with top individuals determining the course of action for the rank and file. The constitutional management emphasizes definite and consistent concern for policies and procedures in dealing with the working group. A line towards a democratic and participative approach follows as employees receive higher education.
- Class and Status System: from a sociologist’s point of view, managers become an elite group of brains and education. This class is based on education and knowledge. Managers continue to expand their horizons in an effort to attain the ultimate in life or goal.
Theories of Management
Scientific Management Theory
Frederick W. Taylor, the “father of scientific management”, postulated that workers could be taught “one best way to accomplish a task”, and that productivity would increase. He called these principles scientific management. This theory employs four principles:
- Traditional “Rule of Thumb”: work organization must employ scientific methods. Workers must be given an adequate amount of time in accomplishing their task.
- Workers can be hired, trained, and promoted based on their competence and abilities.
- Employees are entitled to receiving financial rewards, and incentives for worked accomplishments because Taylor viewed humans as “economic animals” motivated solely by money.
- Maintain good interpersonal relationships between workers and managements. They should be cooperative and interdependent, with the work shared equally.
Taylor’s system of work improvement utilized the following steps:
- Controlled observation of the worker’s performance through time and motion studies
- Scientific selection of the best workers for each job, and training for the job task.
- Paying the worker to a differential rate
- Appointing a few of the most highly skilled workers as managers to plan and prepare the task of workers.
- Appointing foremen (supervisors) for each aspect of the work.
Gilbreth’s Job Simplification
Frank Gilbreth and Lillian Gilbreth (the “first lady of management”) were among the first to use motion-picture films to analyze worker’s motion. They emphasized the benefits of job simplification and the establishment of work standards, as well as the effects of the incentive wage plans and fatigue on work performance.
Gantt Charting
Created by Henry Gantt, a student of Taylor, a Gantt chart is a timeline for tracking aspects of a project. Gantt advocates for humanitarian management, and is concerned with problems of efficiency. He contributed to scientific management by refining previous work rather than introducing new topics.
Classical Organization Theories
Fayol’s Principles of Management and Management Process
Also read: Management Process
Henry Fayol is known as the “father of the management process school”. He studied the functions of the managers and concluded that management is universal. There are fourteen principles of management:
- Division of work
- Authority and Responsibility
- Discipline
- Unity of Command
- Unity of Direction
- Subordination of Individual Interest to General Interest
- Remuneration of Personnel
- Balance of Centralization and Decentralization
- Scalar Chain/Chain of Command
- Order
- Equity
- Stability of Tenure of Personnel
- Initiative
- Esprit de Corps (Team Spirit)
The management process consists of:
- Planning: the determination of philosophy, goals, objectives, policies, procedures, and rules.
- Organizing: establishing the organizational structure to carry out plans, e.g. determining the most appropriate type of patient care delivery.
- Staffing: recruiting, interviewing, hiring, and orienting staff
- Directing: motivating, conflict resolution, delegating, communicating, and collaborating.
- Controlling: performance appraisals, fiscal accountability, quality control, legal and ethical control.
Max Weber’s Types of Authority
The father of organizational management. Webber conceptualized three types of authority:
- Traditional Authority: legitimacy based on long-standing cultural traditions e.g. monarchies.
- Charismatic Authority: authority produced as a by-product of extraordinary personality and charisma.
- Rational Authority: power based on legislature and established rules and regulations.
Lyndall Urwick’s Organizational Theory
She combined the theories of Taylor and Fayol to develop the classic organizational theory. She popularized the term “span of control and unity of command”
Human Relation Management
- Mary Parker Follett (1926) is one of the first theorists to suggest basic principles of what today would be called participative decision making or participative management. She believed that managers should have authority with one another, rather than over employees. She postulates that this leads to better solution-finding and greater employee satisfaction without dominating one or the other.
- Elton Mayo and his Harvard associates conducted a study done at the Hawthorne Works of the Western Electric Company near Chicago, where they found that special attention given to workers results in increased productivity, regardless of environmental conditions. Because of its location, this change in behavior when an individual is aware they are being observed is called the Hawthorne Effect, which is also an important consideration in research.
- Jacob Moreno developed a system of pairings called Sociometry, which states that people are either attracted to, repulsed by, or simply indifferent with other individuals. Often this is done simply by surveying each individual which coworker they would prefer (or not prefer) to work with.
Behavioral Science
- Abraham Maslow developed the Hierarchy of Needs, which states that individuals will only focus on higher level needs when lower level needs are satisfied.
- Physiologic Needs > Safety and Security Needs > Love and Belonging Needs > Self-Esteem Needs > Self-Actualization
- Frederick Herzberg developed the Motivator-Hygiene Theory, a theory that identifies motivators which increase satisfaction and productivity; and hygiene factors which do not produce satisfaction, but is required to avoid dissatisfaction.
- Motivators: achievement, recognition, advancement, creativity, variety, independence, interesting work, responsibility, accomplishment, personal development, interpersonal relationships, status
- Hygiene Factors: salary and benefits, job security, work environment, job policies, supervisory practices, company policies and administration, company reputation
- William Ouchi developed Theory Z, by comparing Japanese organizations to American organizations. It is a blend of both management philosophies.
- Douglas McGregor (1960) theorizes that managerial attitude may be related to employee satisfaction. There are two contrasting theories; Authoritarian (Theory X) and Participative (Theory Y).
- If team members dislike their work and have little motivation, an authoritarian approach may be used. This may involve micromanaging and a “hands-on” position.
- If team members take pride in their work and see it as a challenge, a participative approach may be used. Trust in the members is required.
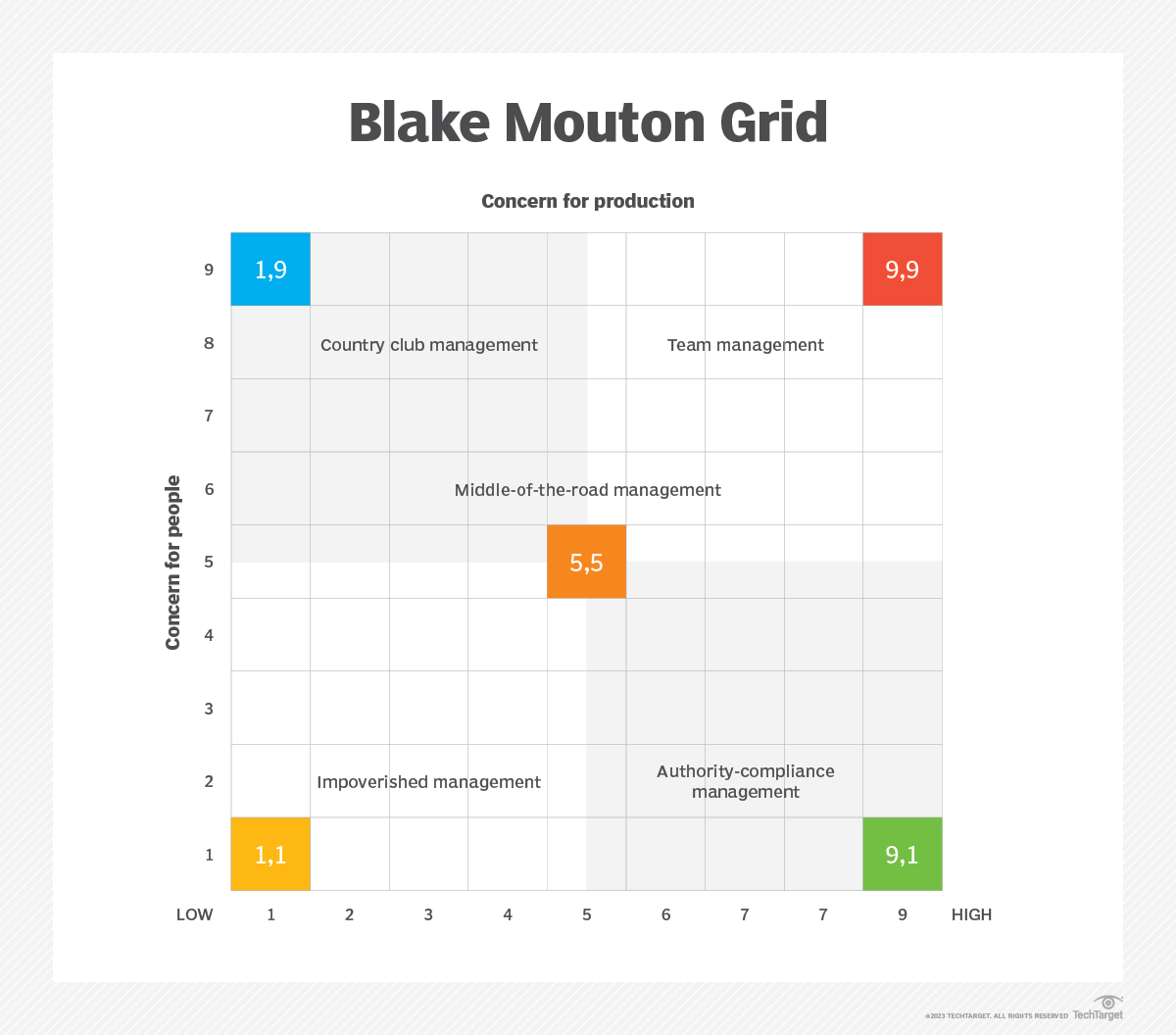
- William Blake’s Managerial Grid is a graph to allow for managers to determine their management style. The two axes of the graph denote concern for productivity (horizontal) and concern for people (vertical). It is divided into four quadrants, named according to their styles:
- Impoverished Management: A low concern for both productivity and people. It is the most ineffective in meeting people’s needs and generating positive results for the organization. Disharmony and conflict arise.
- Country Club Management: A low concern for productivity, but high concern for people. They trust people to manage themselves, so they may not provide adequate direction and coaching. Productivity may suffer, but they believe happy people will work hard and generate good results for the company.
- Authority-Compliance/Produce-or-Perish Management: A high concern for productivity, but low concern for people. Impressive results may be reached using strict rules and punitive measures, but these adversely affect team morale and motivation, eventually resulting in a decline in quality and timeliness of desired results.
- Middle-of-the-Road Management: A moderate concern for both productivity and people. A lack of prioritization for either aspect may result in ineffectivity.
- Team Management: A high concern for both productivity and people. A positive work environment where people feel respected, seen, and heard is created. The workers are motivated and inspired to give their best effort, and productivity improves. Absenteeism and turnover is also reduced in this management style.
Contemporary Management
- A contemporary approach denotes new, recent, or current approaches in a field of management, e.g. a “contemporary approach in steel manufacturing management” may refer to approaches used by other steel companies in the present day.
- A contingency approach gives way for differences between organizations and situations (contingencies) and thus different approaches to management. It assumes there is no single way to best manage a system. The environment impacts the organization, and managers must be flexible to consider environmental changes. The way the organization and control systems are created depends on the environment. A common aspect of the environment that changes frequently and rapidly is technology. Contingencies include:
- Circumstances in the organization’s external environment
- The internal strengths and weaknesses of the organization
- The values, goals, skills, and attitudes of managers and workers in the organization.
- The types of tasks, resources, and technologies the organization uses.
- A systems approach views an organization as a set of interrelated and interdependent parts arranged in a manner that produces a unified whole. It also follows the principle of “there is no one best way to manage”.
- Closed System: systems that are not influenced by, nor interacts with the environment.
- Open System: systems that interact with their environment.
Levels, Skills, and Roles of a Manager
There are various levels of management:
- Top-Level Manager: an individual who looks at the overall operation of the organization. They coordinate internal and external affairs of the organization; makes major decisions; determines the organization’s vision and vision statement, philosophy, policies, and procedures; and creates goals and allocates resources.
- Middle-Level Manager: coordinates activities of different departments. They receive policies from the top-level manager, and makes specific objectives and programs.
- First-Level Manager: directly acts for the actual production of services, acting as links between higher-level managers and non-managers.
A manager should have these skills according to Robert L. Katz (Katz’s Three Skills):
- Technical Skill: knowledge and proficiency for methods, procedures, and processes.
- Human Skill: ability to work with other people for a harmonious working relationship.
- Conceptual Skill: ability to see the overall picture, identify important elements, and their relationships; identifying pertinent factors; and responding to big problems.
Summer also puts forth the following factors:
- Knowledge Factor: ideas, concepts, or principles that can be expressed and are accepted through logical proofs.
- Attitude Factor: beliefs, feelings, and values that may be used on emotions and may not be subjected to conscious verbalization.
- Ability Factor: skill, art, judgment, and wisdom; abstract factors that can direct one’s thinking to factors that can be developed by the individual manager who takes time to consider them.
Managers take on various roles:
- Interpersonal Role: the manager takes on a position as a:
- Symbol: the leader occupies and consists of such duties e.g. signing papers and documents required by the organization.
- Leader who hires, trains, encourages, fires, remunerates, and judges.
- Liaison Officer between outside contacts e.g. the community, and suppliers
- Informational Role: the manager handles information and its distribution, and acts to:
- Disseminate information from external and internal sources
- Monitor information
- be a Spokesperson or representative of the organization
- Decisional Role: a manager takes on the responsibility of decision making, acting as a:
- Problem Solver/Troubleshooter, handling unexpected situations such as resignation of subordinates or loss of clients.
- Innovator/Entrepreneur to improve projects; directs and controls changes in the organization.
- Negotiator in conflict states.
Nursing Leadership
A job title alone does not make a person a leader. Only a person’s behavior determines if they hold a leadership role. While the manager brings things about, the leader influences and guides. There are various definitions for leadership:
- A process of influence in which the leader influences others towards goal achievement.
- The process of influencing the activities of an organized group in its efforts toward goal setting and goal achievement.
- Leadership is about creating change. It involves establishing a direction, aligning people through empowerment, motivating and inspiring them toward producing useful change and achieving the mission.
- Leadership is the vital ingredient that transforms a crowd into a functioning, useful organization.
In the context of Nursing,
Nursing leadership is the process whereby a nurse influences one or more persons to achieve a specific goal in the provision of quality nursing care.
Theories of Leadership
Great Man Theory
This theory simply states that some people are as leaders, and that great leaders arise when the situation demands it. Leaders display both instrumental (technical) and supportive (socially oriented) leadership behavior. Those who lack the ability to be a “great man” cannot adequately develop the necessary traits for leadership.
Trait Theory
This theory advocates that specific traits create a leader. Identified traits include energy, affection, enthusiasm, ambition, aggressiveness, decisiveness, self-assurance, self-confidence, friendliness, affection, honesty, fairness, loyalty, dependability, technical mastery, and teaching skill. This theory allows for individuals to have both inherent and learned traits, deviating from the Great Man Theory.
Charismatic Theory
This theory attributes leadership to charisma; charm; referent power, an inspirational quality that some leaders possess that makes others feel better in their presence.
Situational Theory
- Degree of interpersonal contact possible
- Time pressures
- Physical environment
- Organizational structure
- Influence of the leader outside the group
- Nature of the organization
Contingency Theory
Created by Fred Fiedler in the 1960s, this theory also states no single leadership style is ideal for every situation. Similar to the Situational Theory, it believes the situation changes the leadership style required based on three aspects:
- Leader-Member Relations: assessed through the Group Atmosphere Scale, a Likert scale from 1 to 8 between the following:
- Friendly, Unfriendly
- Accepting, Rejecting
- Satisfying, Frustrating
- Enthusiastic, Unenthusiastic
- Productive, Non-productive
- Warm, Cold
- Cooperative, Uncooperative
- Supportive, Hostile
- Interesting, Boring
- Successful, Unsuccessful
- Task Structure: graded from high to low based on how easy it is to define and measure a task (high). Four criteria are used to determine the degree of task structure:
- Goal Clarity
- Extent to which a decision can be verified by knowing who is responsible for what
- Multiplicity of Goal Paths
- Specificity of solutions, and number of correct answers
- Position Power: the authority inherent in the leader’s position, including the ability to use rewards and punishment.
Fielder provides some leadership styles to match situations:
- If the leader is disliked, but the task is structured, then utilize a diplomatic leadership style.
- If the leader is liked, but the task is ambiguous, then seek cooperation.
- The accepting, considerate leadership style will probably be the most productive in situations with good relations, structured tasks, and position power is either strong or weak.
- In an emergency, a task-oriented leader would be advisable in a natural disaster, as leader-member relations are not a priority.
- In blue-collar work, a relationship-oriented leader may be more productive as the workers often know what to do; have a highly organized task structure.
Leadership Styles (Hersey and Blanchard)
- Directing Style: a high-task, low-relationship style effective when subordinates are low in motivation and ability.
- Coaching Style: a high-task, high-relationship style effective when subordinates have adequate motivation but low ability.
- Supporting Style: a low-task, high-relationship style effective when subordinates have adequate ability but low motivation.
- Delegating Style: a low-task, low-relationship style effective when subordinates are very high in ability and motivation. Similar to laissez-faire leadership.
Path-Goal Theory
This theory states that people act as they do because they expect their behavior to produce satisfactory results. The leader must take charge and set a path to a goal, allowing workers to be more productive and successful.
Transactional Theory
This theory gives emphasis to written or documented policies, rules, and regulations in influencing a group. The needs of followers are identified and the leader provides rewards to meet those needs in exchange for expected performance. Leaders who utilize a transactional method focus on day-to-day operation.
Transformational Theory
This theory gives emphasis to inspirational, motivational, and optimistic leadership in influencing a group. This promotes employee development, attends to the needs and motives of followers, promotes a change in perception, creativity, and provides intellectual stimulation.
Behavioral Theory
This is a management philosophy that evaluates leaders according to the actions they display in the workplace; to be an effective leader is to learn a certain set of behaviors. This shifted focus away from the traits of the leader to the actions of the leader.
Leadership Styles (Kurt Lewin)
Lewin along with White and Lippitt identified the following common leadership styles:
- Authoritarian Leadership: a leader who uses positional and personal power who is demanding and controlling. They emphasize differences in status and directs or commands others. Criticism is punitive, and communication is vertical. Decisions are made based on their opinion alone.
- Democratic/Participative Leadership: a leader who allows for group governance through collaboration or group efforts. It requires trust and openness, and less control is maintained. Both economic and ego rewards are used to motivate, and emphasis is placed on “we” rather than “I and you”. Criticism is constructive.
- Laissez-Faire Leadership: a “hands-off” approach to leadership, often with poor results. Informal leaders arise in a somewhat-decentralized manner for the group. Leaders are uninvolved, disinterested, withdrawn, and permissive. They do not provide criticism, and allows their subordinates to plan.
Servant Leadership
These leaders are more concerned with the needs of others than themselves, and lead through their service. They foster a service inclination in others that promotes collaboration, teamwork, and collective activism.
Authentic Leader
A leader manager arsenal; in order to lead, leaders must be true to themselves and their values, then act. Authentic or congruent leadership theory differs from the traditionaltransformational leadership theory.
Thought Leader
This applies to a person who is recognized among their peers for innovative ideas and demonstrates the confidence to promote these ideas.
Power
Power is the ability to impose the will of one person or group to bring certain behaviors to other persons or groups. Power may take various forms:
- Rewarding Power: the power to reward workers for their performance; to compensate or remunerate the achievements of the staff e.g. bonuses, awards, promotions
- Coercive Power: the use of fear or duress to gain control; the opposite of rewarding power e.g. reprimands, termination, penalties
- Legitimate Power: power conferred upon a leader based on organizational definitions of authority; power vested upon a leader in relation with their position or rank sanctioned by the institution itself.
- Referent Power: power attained from the ability of the leader to obtain admiration; based on charisma.
- Expert Power: power based on the knowledge, skills, information, and expertise of the leader in the domains they oversee. This gains respect and compliance.
- Information Power: power based on access to knowledge, access to information, and communication avenues (e.g. memos). It is especially powerful when others require pertinent information, such as recent changes in healthcare standards.
- Connection Power: power based on access and familiarity with other influential individuals.
Patient Health Care Delivery System
The Nursing Process is used in the delivery of nursing care service. It follows the ADPIE format: Assessment, Diagnosis, Planning, Intervention, Evaluation.
Patient Classification System
As the name suggests, a PCS (A.K.A. Workload Management, Patient Acuity Tools) groups patients according to their acuity of illness and the complexity of necessitated nursing activities. The totality of projected nursing needs for the succeeding shifts is typically based on patient acuity data, collected every shift. Using the PCS provides an objective approach to determine staffing based on patient care needs. Basically, the more sick people, the more nurses required.
Barriers
Barriers to the use of PCS include the lack of standardization, a lack of credibility, and a lack of consideration for patient flow (Hertel, 2012).
| PCS Acuity or Level of Care | Nursing Care Hours Required |
|---|---|
| Level 1: Self-Care or Minimal Care | 1.5 |
| Level 2: Moderate or Intermediate Care | 3.0 |
| Level 3: Total or Intensive Care | 4.5 |
| Level 4: Highly Specialized or Critical Care | 6.0 or 7.0 hours or more |
- Level 1: patients who are recovering, often requiring only diagnostic studies, minimal therapy, less frequent observations, and daily care for minor conditions and are awaiting elective surgery.
- Level 2: moderately ill or recovering from serious illness or an operation. They require nursing supervision or assistance that is related to ambulating and caring for their own hygiene.
- Level 3: patients need close attention and complete care all throughout the shift. The nurses initiate, supervise, and perform most of the patient’s activities.
- Level 4: acutely ill patients with a high level of nurse dependency
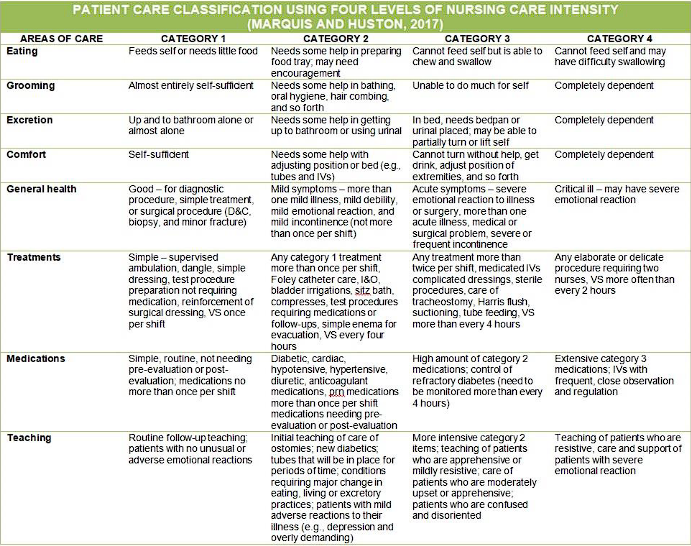
Patient classification systems are institution-specific and must be modified to reflect the unique staff and patient population of each organization. Maybe other variables also make it difficult to simply transfer a PCS from one facility to another. Here’s one example (too much info that I don’t think will be relevant given the preceding statement):
Modalities of Care
Caregiving in an organization will naturally require some method of labor division and assignment. In the field of nursing, there are five well-known methods for organizing patient care:
| Method | Basic Principle |
|---|---|
| Case Method Nursing | ”Total Patient Care”. The oldest; patients are assigned as cases to nurses, who take total responsibility for their needs. |
| Functional Nursing | Task-based assignment based on nurse competence and specialty. |
| Team Nursing | A professional nurse coordinates ancillary personnel to provide care to a group of patients. |
| Modular Nursing | A refined form of team nursing, forming smaller teams or even pairs of at least one registered nurse. |
| Primary Nursing | ”Relationship-based nursing”. A primary nurse assumes responsibility for planning the care patient/s from admission to discharge. |
| Case Management | Highly individualized care created from a collaborative process of assessment, planning, facilitation, and advocacy by case managers. |
| Case Method Nursing or Total Patient Care Nursing is the oldest mode of organizing patient care. Nurses assume total responsibility during their time on duty for meeting all needs for assigned patients. Planning is less necessary, and the lines of responsibility and accountability are clear. |
- Pros: the nurses receive high autonomy and responsibility, allowing for holistic and unfragmented care during the nurse’s shift.
- Cons: care may become fragmented between shifts, there is less efficiency as the specialized nurse performs tasks that could be delegated instead, and most importantly, the necessitated competency on nurses to handle autonomy— inexperienced nurses may fail to provide total care for the patient.
Functional Nursing evolved from the great shortage of nurses after the second world war. Relatively untrained workers were trained to perform simple tasks and gained proficiency by repetition. Personnel are assigned to tasks rather than patients, e.g., a nursing aide handles all vital signs monitoring, one registered nurse handles all the medications required, etc.
- Pros: high efficiency in times of high demand, accommodating for many levels of competency. Nurses become managers of care rather than direct providers.
- Cons: care is fragmented, and patient needs may be overlooked. Job satisfaction may also be low. The need for many care coordinators may increase costs.
Team Nursing handles a group of patients under the supervision of a professional nurse (often chosen democratically) who shares responsibility in care. The team leader must know the condition and needs of all the patients for planning individual care. The role of the team leader can vary, from coordinating patient activities to giving direct personal care to patients.
- Cons: an extensive amount of communication is required, and teams are limited to ≤5 people, as large teams will revert to functional lines of organization. The team leader requires excellent communication and organizational/leadership skills to properly implement this type of care.
Modular Nursing is a refined form of team nursing, as team nursing was mostly never practiced in its purest form. Modular nursing changes this by forming smaller teams (mini-teams, care pairs— 2 or 3 people) with at least one registered nurse. These teams are often assigned geographically.
- Pros: a smaller team requires less coordination and communication, allowing more time for direct patient care activities.
Primary Nursing, also known as relationship-based nursing, was developed in the late 1960s. It takes from Total Patient Care and involves bedside care: the primary nurse assumes 24-hour responsibility for planning the care of assigned patients from admission to discharge. This care is provided directly by the primary nurse during their shift, and followed by associate nurses otherwise.
- Pros: clear interdisciplinary group communication and consistent, direct patient care by relatively few nursing staff allows for holistic, high-quality patient care. Additionally, this type of nursing can be applied in other contexts, e.g., hospice care, home nursing. Job satisfaction is also high, as nurses feel challenged and rewarded.
- Cons: improper implementation fails to coordinate a multidisciplinary team or fails to identify complex patient needs and changes in condition. High experience and skills are necessary for this role.
Case Management is a collaborative process of assessment, planning, facilitation, and advocacy for options and services to meet an individual’s health needs through communication and available resources to promote quality cost-effective outcomes. This process, handled by the case manager, often uses critical pathways and multidisciplinary action plans (MAPs) to plan patient care; the Care MAP is a combination of a critical pathway and a nursing care plan.
- Pros: each patient is considered individually to identify the most cost-effective care setting possible. Community resources, providing healthcare information, and testing and procedures are all included in care.
- Cons: being a case manager requires extensive knowledge and experience. This role is argued to be reserved for advance practice nurses or those with advanced training.
Contemporary Models of Care
| Model | Basic Principle |
|---|---|
| Professional Nursing Practice Model | A framework for guiding and aligning clinical practice, education, administration, and research in order to achieve positive patient and nurse staff outcomes. This is a core feature of magnet hospitals. |
| Differentiated Nursing Practice Model | The provision of care is differentiated according to the level of competency of the RN, scaling responsibility with expertise. |
| Clinical Nurse Leader Model | A clinical nurse leader (CNL) designs, implements, and evaluates patient care by coordinating an interprofessional team in the provision of care. They are a provider and coordinator of care (rather than a manager and leader) and fosters inter- and intraprofessional communication. |
| Synergy Model for Patient Care | ”Synergy” occurs when the needs and characteristics of the patient, clinical unit, and/or system are matched with the nurse’s competencies. |
| Transforming Care at the Bedside | The main goal of this model is to improve patient care and decrease turnover (improve employee retention). It involves five themes: transformational leadership, safe and reliable care, vitality and teamwork, patient-centered care, and value-added care processes. |
| Patient-Centered and Family-Centered Care Model | This model emphasizes the inclusion of patients and their families in collaboration, no matter their age, level of care, and healthcare setting. The patient retains control over their care, and all healthcare decisions are made with the RN as a collaborator. |
Organizational Structure
Fayol postulates that an organization is created once the number of workers begins to necessitate a supervisor. Organizations allow for collective effort, outweighing individual effort.
Venzon (2016) on Organizations
“It pertains to the body of persons, methods, policies and procedures arranged in a systematic process through the delegation of functions and responsibilities for the accomplishment of purpose.”
Organizational structure is divided between formal and informal structure. In formal structure, managerial authority, responsibility, and accountability is clearly defined; roles and functions are outlines, people have specific tasks to perform, and rank and hierarchy are apparent.
On the other hand, informal structure is the channel that “fills in the gaps with connections and relationships that illustrate how employees network with one another to get the work done.” As supported by Schatz (2013) informal structures are typically centered on camaraderie and often produce direct response from individuals, saving time and effort. It is also useful when the formal structure becomes non-effective.
The communication network used for informal structure is grapevine, consisting of exchanges in the break room, in the hall way, in a carpool, in between work, and online that allows relationships of informal groups to develop.
Organizational Theory and Bureaucracy
Revisiting Max Weber, he states that bureaucracy is an institutional method for applying general rules to specific cases, making the actions of management fair and predictable. Other characteristics of bureaucracy include:
- A clear division of labor.
- A well-defined hierarchy of authority, separating superiors from subordinates. There must be remuneration for work, recognition of authority, allotment of privileges and conferring of promotions.
- There must be impersonal rules and impersonality of interpersonal relationships.
- A system of procedures for dealing with work situations must exist.
- A system of rules covering the rights and duties of each position must be in place.
- Selection for employment and promotion is based on technical competence.
To highlight the structure and order of an organization, an organizational chart utilizes a line drawing that diagrammatically shows the formal organizational relationships, areas of responsibility, superiors of subordinates, and channels or organization. In filling out an organizational chart, organizing must take place. It involves the establishment of formal authority and producing structure by identifying groupings, roles, relationships, and staffing patterns. Each role involves job descriptions, qualifications, and functions.
Evidence-Based Practices in Nursing Management
The standards used in nursing complies with the National Nursing Care Competency Standards (NNCCS), an initiative of the PRC-BON. A national task force was formed for the development of core competency standards, completed in 2005.
Foreword (NNCCS, 2012) by PRC Chair T.R. Manzala:
“Out of this lengthy process emerged the Revised Nursing Core Competency Standards, emphasizing the three roles of the nurse: Beginning Nurses’ Role on Client Care, Beginning Nurses’ Role on Management and Leadership and Beginning Nurses’ Role in Research, as well as four types of clients of the nurse. With the promulgation of the 2012 NNCCS, the succeeding stage is its implementation and evaluation in both nursing education and nursing service in all settings. This will be a collaborative activity of all partners of the PRC-BON.”
Goals and Objectives of the Project
The goals of the project are in line with a grant from the International Labour Organization (ILO). The project is entitled the “Nursing Core Competencies for Master Trainers in Nursing Education and Practice”, and was the first step of the 2012 NNCCS. The project aims to:
- Establish a team and system for implementing the project
- Develop and implement the training design and materials aligned with the revised NNCCS competencies
- Pilot the training course in Luzon, Visayas, and Mindanao
- Recommend strategies to address sustainability concerns
Significance
These goals are significant as they serve as the basis for basic nursing education programs through CHED, as a competency-based test framework for the development of course syllabi and test questions for the board exam, as standards of professional nursing practice in various settings, and all related evaluation tools in said settings.
| Phase | Title |
|---|---|
| Phase 1 | Work Setting scenario |
| Phase 2 | Validation studies of roles and responsibilities/Benchmarking |
| Phase 3 | Integrative review of outputs from the validation strategies |
| Phase 4 | Core competency consensual validation |
| Phase 5 | Conduct of public hearing |
| Phase 6 | Promulgation of the revised and modified core competency standards. |
| Phase 7 | Printing of the revised and modified core competency standards. |
| Phase 8 | Training in the implementation of the revised core competency standards. |
| Phase 9 | Implementation of the revised core competency standards. |
| Phase 10 | Evaluation of effectiveness of the revised core competency standards. |
Patient Care Safety Standards
Nurses, as the largest group of healthcare service providers, are vital members of the healthcare team. According to Transforming the Work Environment of Nurses, nurses are the healthcare service professionals most likely to intercept errors and prevent harm to patients. Given this fact, it is imperative for nurses to know what proven techniques and interventions can be used to enhance patient and organizational outcomes. Key elements can avoid harm, and promote effective and safe service:
- Nursing Leadership: leadership and political commitment are essential. The leader addresses strategic priorities for institutional development, its culture, and its infrastructure. They engage with various stakeholders, communicate, and build awareness.
- Institutional Development: approaches to institutionalize patient safety and quality in the health facilities will have to consider:
- Financial and human resources
- Facility and equipment management
- Strengthen management responsibility
- Authority and competency
- Formulate standards of what is expected and communicates such standards and provides training for attaining them
- Enforcing the standards that come with the policies, and giving the patients a voice through a feedback or grievances system (patient satisfaction survey).
- Reporting System: the National Patient Safety Committee shall develop and institutionalize a proactive reporting and learning system that requires its leadership to encourage reporting of events.
- Feedback and Communication: feedback can allow for the institution to benchmark their performance, demonstrating commitment to ensuring continuous improvement.
- Adverse Event Prevention and Risk Management: strategies including risk assessment, patient feedback surveys, health technology assessment, and safety assessment codes are put in place to prevent adverse events.
- Disclosure of Reported Serious Events: the reporting system, while ensuring confidentiality, makes available to the public the results of investigation and summary or annual reports that summarize events and the corresponding actions taken.
- Professional Development: training and supervision of healthcare staff is important in improving clinical judgments and decision-making. The standard norms of behavior (courtesy, promptness, efficiency) is instilled among the healthcare workers to improve the quality of service.
- Patient-Centered Care/Empowerment of Consumers: patient safety initiatives all revolve around the patients. They are partners in all aspects of the process. This is a national priority and core agenda to improve quality care in all health and to protect patients from faulty systems.
These standards for safety in healthcare are important in improving patient satisfactions, outcomes, accuracy in identification, effectiveness of communication, safety in medication, staff productivity, staff retention, occupational health and environmental awareness (Ergonomics). They reduce the risk of healthcare associated infections and harm and injury resulting from faulty service. Workers must be trained and convinced of the methods used for reducing pain and discomfort.
Staff Safety
- Promote a culture of safety: the general attitude of the company influence the working environment. Hospitals that place big emphasis on staff safety are more likely to prevent incidents.
- Measure the performance of safety protocols: record-keeping is used to evaluate the protocols in place. Incidents are reported, and learning from them is critical to implementing staff safety.
- Optimize staff scheduling: when understaffed, employees are overworked and the risk of incidents increases. A balance should be maintained in minimizing labor costs while maximizing staff safety.
- Improve patient handling: handling patients is one of the most physically demanding aspects of nursing.
- Use safer medical equipment: medical devices and recent innovations eliminate health risks that have been constant enemies of care, such as infection control, prevention of needlestick injuries, reducing medication errors, increasing protection against exposure to blood and drugs, and minimizing disconnections, air embolisms, and misconnections.
Patient Safety by Nurses
Nurses should have the proper knowledge and implementation of healthcare policies and procedures. Open communication and teamwork between all other healthcare providers is quintessential in appropriate, cohesive care. More specific actions by nurses to improve patient safety include:
- Reviewing the medication rights before giving the medications.
- Engaging in creating and updating a report system to avoid blaming culture.
- Be involved in research and evidence-based activities for better decision making.
- Be up-to-date on all life-saving certifications (CPR, BLS, ACLS, PALS, NALS) and other Nursing Specialty Certification Programs.
- Engage in hospital committees to advocate for safe, effective, and patient-centered healthcare systems.
- Be responsible in reporting all errors and near misses for the patient and for the prevention of sentinel and adverse events in the future.
- Ensure better lighting and less clutter in work areas.
Sentinel Events and Near Misses
Sentinel events are patient safety events that result in death, permanent harm, or severe temporary harm. Near Miss events are errors that occur in the process of providing medical care that are detected and corrected before a patient is harmed.
Standards of Professional Nursing Practice (ANA)
The standards of professional nursing practice as dictated by the American Nurses Association (2015) is composed of the Standards of Practice and Standards of Professional Performance:
- Standards of Practice: the level of competency a nurse demonstrates with the critical thinking model known as the nursing process (Assessment, Diagnosis, Outcomes Identification, Planning, Implementation, and Evaluation). These encompass significant actions taken by registered nurses and forms the foundation of the nurse’s decision-making.
- Standards of Professional Performance: sixteen outlined key aspects of professional nursing.
| Standard | The Registered Nurse |
|---|---|
| 01: Assessment | …collects comprehensive data pertinent to healthcare. |
| 02: Diagnosis | …analyzes the assessment data to determine the diagnoses or issues. |
| 03: Outcomes Identification | …identifies expected outcomes for a plan individualizes to the client or situation. |
| 04: Planning | …develops a plan that prescribes strategies and alternatives to attain expected outcomes. |
| 05: Implementation | …implements the identified plan. - 05a: Coordination of Care - 05b: Health Teaching and Promotion - 05c: Consultation - 05d: Prescriptive Authority and Treatment |
| 06: Evaluation | …evaluates progress towards the attainment of outcomes. |
| 07: Ethics | …practices ethically. |
| 08: Education | …attains knowledge and competence reflecting current nursing practice. |
| 09: Evidence-Based Practice and Research | …integrates evidence and research findings into practice. |
| 10: Quality of Practice | …contributes to quality nursing practice. |
| 11: Communication | …communicates effectively in all areas of practice. |
| 12: Leadership | …demonstrates leadership in the practice setting and profession. |
| 13: Collaboration | …collaborates with healthcare consumers, families, and others in the conduct of nursing practice. |
| 14: Professional Practice Evaluation | …evaluates their own practice in relation to standards, guidelines, statutes, rules, and regulations. |
| 15: Resource Utilization | …utilizes appropriate resources to plan and provide safe, effective, and financially responsible nursing service. |
| 16: Environmental Health | …practices in an environmentally safe and health manner. |
Ethical, Legal, and Moral Considerations in Nursing Leadership Management
Some parts of this note are copied word-for-word given the nature of legal jargon and phrasing (especially the Preamble). I’ve tried to provide key phrases or words for each section to allow them to be more memorable. Just read the references anyway, it’s not that long.
References
The basis for the code of ethics for nurses was created by the Board of Nursing (BON) in coordination and consultation with the Philippine Nurses Association (PNA) based on the Code of Good Governance for the Professions in the Philippines, and approved by the Professional Regulation Commission (PRC) on July 14, 2004.
Code of Ethics for Nurses
Board Resolution No. 220, Series of 2004 approved last 14th day of July, 2004: the promulgation of the code of ethics for registered nurses.
Article I: Preamble
Section 01 (What?): Health is a fundamental right of every individual. The Filipino registered nurse, believing in the worth and dignity of each human being, recognizes the primary responsibility to preserve health at all cost. This responsibility encompasses promotion of health, prevention of illness, alleviation of suffering, and restoration of health. However, when the foregoing are not possible, assistance towards a peaceful death shall be his/her obligation.
Section 02 (How?): To assume this responsibility, registered nurses have to gain knowledge and understanding of man’s cultural, social, spiritual, physiological, and ecological aspects of illness, utilizing the therapeutic process. Cultural diversity and political and socio-economic status are inherent factors to effective nursing care.
Section 03 (Why?): The desire for the respect and confidence of clientele, colleagues, co-workers, and the members of the community provide the incentive to attain and maintain the highest possible degree of ethical conduct.
Article II: Registered Nurses and People
Section 04: Ethical Principles (for people)
- Respect individual beliefs. This includes values, customs, and spirituality.
- Respect autonomy and self-determination. Individuals are free to make rational and unconstrained decisions.
- Respect confidentiality. Any personal information acquired during care is held in strict confidence.
Section 05: Guidelines to be observed (for care of people)
- Be holistic. Both the individuality and totality of patients are considered when administering care.
- Respect spirituality, culture, and values (again?). Beliefs and practices are respected in regards to diet and treatment. However, in the event of conflicts, their welfare and safety must take precedence.
- Uphold the rights of the individuals.
Article III: Registered Nurses and Practice
Section 06: Ethical Principles (in practice)
- Human life is inviolable.
- Quality and excellence are the goals of practice.
- Accurate documentation of actions and outcomes of delivered care is the hallmark of nursing accountability.
Section 07: Guidelines to be observed (in the practice of nursing)
- Follow the scope of nursing practice as defined by R.A. 9173 (The Philippine Nursing Act of 2002) and Board Res. No. 425, Series of 2003, the Rules and Regulations Implementing the Philippine Nursing Act of 2002 (IRR).
- Be aware of the duties and responsibilities defined in the aforementioned legal bases.
- Become competent in knowledge, skills, and attitude through various learning situations.
- For administrators, provide a favorable environment for growth and development, and minimize ineffective and unlawful practice of registered nurses in their charge.
- Know that specialization programs are accredited through the Nursing Specialty Certification Council (NSCC).
- Strive for the optimum standard of safe nursing practice, and any modifications from the standard should follow the principles of safe nursing practice.
- Maintain confidentiality for the patient, allowing only those professionally and directly involved in their care to view records or when required by law.
Section 08: Ethical Principles (for patients’ rights)
- Nurses are advocates. They safeguard patient rights and privileges.
Section 09: Guidelines to be observed (in upholding rights):
- Respect the Patients’ Bill of Rights. In particular, provide the patient or their families information (4th in the patients’ bill of rights). All pertinent information except those deemed harmful is provided. If conflicts arise, the patients’ rights area upheld.
Section 10: Registered nurses should be aware that there are professional, ethical, moral, and legal dimensions in their actions. They strive to perform their work in the best interest of all concerned.
Section 11: Prohibitions and Regulations
- Follow existing laws, rules, regulations, measures, and generally accepted principles of moral conduct and proper decorum in professional duties.
- Do not demean the image of the profession in advertisements, such as in indecent exposure, dress code violations, seductive behavior, etc.
- No gifts, favors, or hospitality that can be interpreted as capitalizing on patients should be declined.
- Referrals should not be capitalized upon. Any demands or reception of any commission, fee, or emolument for recommending or referring a patient to other healthcare professionals is prohibited.
- No abuse of the privileged nurse-patient relationship should take place, such as access to property, resident, or workplace.
Article IV: Registered Nurses and Co-workers
Section 12: Ethical Principles (in working with others)
- Maintain solidarity with other members for the patient’s best interest.
- Maintain a collegial and collaborative working relationship.
Section 13: Guidelines to be observed (in working with others)
- Nurses must maintain their professional role/identity when working with others.
- Nurses must conform with group activities based on acceptable, ethicolegal standards.
- Nurses must contribute to professional growth and development of other members of the health team.
- Nurses must actively participate in professional organizations.
- Nurses must not act in any manner prejudicial to other professions.
- Nurses must honor and safeguard the reputation and dignity of nurses and other professions. Avoid unfair and unwarranted comments or criticisms on competence, conduct, and procedures.
- Nurses must respect the rights of their co-workers.
Article V: Registered Nurses, Society, and Environment
Section 14: Ethical principles
- The preservation of life, respect for human rights, and promotion of health environment shall be a commitment of the Registered Nurse.
- The establishment of linkages with the public in promoting local, national, and international efforts to meet health and social needs of the people as a contributing member of society is a noble concern of a Registered Nurse.
Section 15: Guidelines to be observed
- Nurses must be conscious of their obligations as citizens, i.e. be involved in community concerns.
- Nurses must be equipped with knowledge of health resources within the community, and take an active role in primary health care.
- Nurses must actively participate in programs, projects, and activities that respond to the problems of society.
- Nurses must lead their lives in conformity with the principles of right conduct and proper decorum.
- Nurses must uplift the nursing profession at all times with their image.
Article VI: Registered Nurses and the Profession
Section 16: Ethical Principles (in the nursing profession)
- Maintenance of loyalty to the nursing profession and preservation of its integrity are ideal.
- Compliance with the by-laws of the accredited professional organization (PNA), and other professional organizations of which the Registered Nurse is a member is a lofty duty.
- Commitment to continual learning and active participation in the development and growth of the profession are commendable obligations.
- Contribution to the improvement of the socio-economic conditions and general welfare of nurses through appropriate legislation is a practice and a visionary mission.
Section 17: Guidelines to be observed (in the nursing profession)
- Be members of the PNA (the accredited professional organization)
- Strictly adhere to nursing standards
- Participate actively in the growth and development.
- Strive to secure equitable socio-economic and work conditions in nursing through appropriate legislation and other means.
- Assert for the implementation of labor and work standards.
Article VII: Administrative Penalties, Repealing Clause, and Effectivity
The Certificate of Registration of Registered Nurse shall either be revoked or suspended for violation of any provisions of this Code pursuant to Sec. 23 (f), Art. IV of R. A. No. 9173 and Sec. 23 (f), Rule III of Board Res. No. 425, Series of 2003, the IRR.
Also read: Nursing Accountability by Luansing
International Code of Ethics for Nurses
With its latest revision being in 2012, the International Council of Nurses (ICN) has also adopted an international code of ethics:
- Nurses and the People: the main professional responsibility of nurses is to people requiring nursing care.
- Nurses and Practice: the nurse carries personal responsibility and accountability for nursing practice, and maintains competence by continual learning
- Nurses and the Profession: the nurses have major roles in determining and implementing acceptable standards of clinical nursing practice, management, research, and education. They are also active in developing a core of research-based professional knowledge, and of professional values.
- Nurses and Co-workers: the nurse sustains a collaborative and respectful relationship with co-workers in all fields. They take appropriate action to protect individuals, families, and communities if their health is endangered by a co-worker or any other person. Similarly, the nurse supports and guides co-workers to advance in ethical conduct.
Contracts
A contract is a meeting of minds between two persons where each party binds themselves to the other, to give something or to render some service. It is a promise or a set of promises which the law recognizes as a duty which, if unfulfilled, the law remedies. In nursing, when a nurse enters into a contract with an employer, it often entails a salary and a set of benefits in exchange for their services as a nurse. Contracts can take various forms:
| Contract | Definition |
|---|---|
| Formal Contract | A contract put into writing by some special laws. This includes marriage contracts, mortgages, deeds of sale, work contracts, etc. |
| Informal Contract | A contract put into writing without an involvement of the law, or those produced by oral or spoken discussion with evidence and intention to form a contract. |
| Voidable Contract | A contract that can be retracted if fraud or misrepresentation has been involved in its formulation, especially in the absence of free consent from one or more involved parties. This contract is non-binding. |
| Void Contract | A contract that has ceased to be enforceable, either from its conception or from a change in events or circumstances. The name “void contract” is a misnomer; a contract does not exist if it is void. In this case, it should be referred to as a “void agreement”. |
| Unenforceable Contract | A contract that the law cannot enforce, such as void contracts, unconscionable contracts, impossible contracts, and contracts against public policy. It may be valid between the parties, but will not be enforced by the law. |
| Executed Contract | A contract where both parties have performed their obligation. |
| Executory Contract | A contract yet to be executed; a contract where neither party has fulfilled their obligation. For example, a contract for a medical procedure is executory if the procedure nor the payment has been carried out. |
| Express Contract | When a contract’s terms are reduced in writing or are agreed upon by spoken words at the time of its formation. “Express” in this case refers to the shortening of the process. |
| Implied Contract | The terms of a contract which are implied based on the conduct or dealing between the parties. For example, the patient consenting to the administration of medications also consent to the method (even if invasive) by which those medications are given. |
| Quasi-Contract | A legal obligation decided by a judge for one party to compensate the other, such as in the case of a medical procedure being carried out by party A, but not being paid for by party B. In this case, a quasi-contract for party B to fulfill their obligation through their property is produced by a judge. |
| Contingent Contract | A contract set in place as a contingency. For example, a payment will be made to a worker in the event that the worker suffers an injury at a workplace. |
| Inexistent Contract | Contracts that are void or inexistent from the beginning, either due to unlawful terms, with invalid causes, whose object is outside the commerce of man, whose service is impossible, where the intention in relation to the principal object cannot be certain, those who are declared void by law, or those who are fictitious or simulated. |
| Voidable Contract | Contracts wherein one of the parties are incapable of giving consent, and those whose content is vitiated by mistake, violence, intimidation, or undue influence or fraud. |
| Illegal Contract | Contracts fraudulently, unlawfully, or prohibitively produced. |
A contract, being bound by the law, has various requisites before its validation:
- The presence of two or more consenting parties.
- Consent requires legal capacity dictated by age and sound mind (freedom from intoxication, duress, or mental disability).
- Married couples may need to enter into contracts with both parties involved; some contracts require both husband and wife to sign into a contract, such as in a mortgage.
- The object which is the subject matter of the contract is specified. Said object must not be outside the commerce of man, not untransmissible, future inheritance only within the authority of law, and do not contradict the law, morals, good customs, public order, and public policy.
- The cause for obligation should be established. Time, price, and subject are expressed.
- Generally, the duration of the contract is at least as long as the shortest fulfillable obligation, such as in salaries— a yearly salary will entail a contract valid for at least one year.’
Written contracts are often feared by personnel, and prefer oral contracts instead. However, a written contract includes many advantages:
- Certainty. Written contracts are certain and avoid issues with human memory.
- Time Frame. Written contracts contain a set time frame of validity as to protect both sides against sudden changes without notice.
- Setting Standards. An individual no longer needs to haggle for the amount of compensation to receive or to give, as all details is outlined within the contract. This also sets definite standards between contracts between different parties, to avoid favoritism.
- Procedure Setting. A written contract can outline the definite procedure to follow, especially for cases of complains of substandard work. The employer provides a clear course of action and the professional nurse has protection against arbitrary action. A nurse’s accountability for a negative outcome is reduced if such actions that resulted to the outcome has been outlined within a contract.
- Commitments are defined in a written contract, such as hours of work, salary, time of validity, days off duty, and reprimands in the case of unfulfillment of the terms of the contract.
Breach of Contract
A breach of contract occurs when there is a failure to perform the obligations set within an agreement, whether expressed or implied, without cause. The following are what constitute breaches of contract in nursing services:
- Prevention of performance
- Failure to perform because of inconvenience or difficulty; failure of cooperation in performance;
- Abandonment of duty (e.g., leaving unconscious patients, going off-duty without endorsement, loafing while on-duty)
- Substitution of Performance
- Failure to use due care
However, there are instances where refusing, neglecting, or failing to perform a contract is legally excused:
- Discovery of material misrepresentation made and relied upon;
- Where performance would be illegal, impossible (e.g. by reason of illness, death of patient or nurse, etc.), and where the contract is insufficient (lacking one or more elements to make it valid).
Wills
A will is a legal declaration of a person’s intentions upon death. It is called a testamentary document, as it occurs after the death of its maker. It is an act where a person is permitted by the law to control the deposition of their estate to take effect after death.
- Holographic Will: a will that is written, dated, and signed by the hand of the testator themself. In this type of will, at least one witness who knows the handwriting and signature of the testator explicitly declares that the will and the signature are in the handwriting of the testator.
- Oral Wills, Nuncupative Wills, Deathbed Wills: wills not put into writing, usually made in the presence of witnesses. The testator will say out loud to someone else how they wish for their property and assets to be distributed after their death.
- At least two witnesses are required for a nuncupative will.
- The following restrictions apply: the transcription of an oral will into writing is done at the time of their last illness at the place in which they died, within a given number of days and that it be offered to probate (the legal process of validation and administration of wills) within a specified time.
The creation of a will follows several legal requirements:
- The testator must have the expressed intention of making a will, be of the right age (18+) and of sound mind, and be free from undue influence.
- The testator shall name the person in charge of carrying out the provisions of the will.
- Properties, if disposed, should follow their respective legal requirements.
- The will must be signed by the testator, and attested and signed by at least three witnesses in his presence and of one another. Every witness shall be of sound mind, 18 years of age or more, not blind, deaf or dumb, and able to read and write.
- Every will must be acknowledged before a notary public by the testator and witnesses.
- A married woman may make a will without the consent of her husband and without the authority of the court.
Nursing Obligations in a Will
A nurse verifies the client as being of age, of sound of mind and free from fraud or undue influence. The nurse notes that the will was signed by the testator, and that all witnesses were present simultaneously and signed the will in the presence of the testator.
Gifts
Gifts are a form of property disposal besides the creation of a will. These consist of personal property, with the indication of the transfer of control over such property, and with the acceptance of the recipient. These gifts, when made in the anticipation of death, are called Gifts Causa Morta or Donation Causa Mortis.
Legal Procedure and Trial
The following is a summary of legal procedures a nurse may become involved in. A trial works to ascertain facts by hearing relevant evidence, applying the appropriate principle of law, and passing judgment:
- Commencement of the Action: the first step to take is to determine the type of legal action to take, such as negligence for negligence, and breach of contract for a failure to fulfill contractual obligations.
- Statutes of Limitation: complaints must be made within a specific time or the right to complain may be lost forever. There is a time limit in filing cases because witnesses become less reliable after the passage of time. In claims for negligence or malpractice, the limit may vary from 2 to 3 years. In criminal cases, the limit may vary from 2 to 6 years, except in the case of murder, in which there is no time limit.
- Pleading: also known as indictments, each party produces statements of facts, or “pleads” to the court. The First Pleading is generally known as the complaint or petition. In less serious crimes, these are misdemeanors. In more serious crimes, they are felonies.
- Pre-Trial Procedures: an informal discussion between the judge and attorneys to eliminate matters not in dispute, agree on issues, and settle procedural matters relating to the trial. Cases often become settled at this point without reaching trial.
- Trial: the facts of the case are determined, the principles of law are applied, and a conclusion as to liability is reached, as determined by the judge.
- Witnesses: the necessity of testimony by a person in a legal proceeding as determined by the attorneys for the parties involved.
- Subpoena: a court summons, directing a witness to appear and give testimony on the date and time ordered.
- Subpoena duces tecum: a subpoena requiring the addition of records, papers, and the like which may be in their possession and will be pertinent to the issue.
- Testimony of opinion: the opinion of expert witnesses qualified to testify based on special knowledge, skill, experience, and training.
- Ante-mortem statements or dying declarations are considered hearsay, except when stated by a victim of a crime.
- Appeals: if an appeal against a complaint is desired, an appellate court reviews the case and forms a final judgement, and the matter is ended.
- Execution of Judgement: generally, lawsuits against hospitals or healthcare workers involve monetary reimbursement for damages. The defendant is compelled to execute the judgement, or is held in contempt of court if they are not to comply. In such a case, a fine or imprisonment may be imposed.
Telephone Orders
Telephone orders are only to be used in extreme emergency when there is no alternative. The use of telephones for orders can lead to serious errors and border on malpractice. Confirmation and double-checking if a received order is correct is done and written on the patient’s chart, with the nurse’s signature and the physician’s name to be countersigned by the physician at the next visit within 24 hours.
Consent in Health Care
Consent is defined as a free and rational act that presupposes knowledge of the thing to which consent is being given by a person who is legally capable of giving consent. Specifically, informed consent is an established principle of law that every human being of adult years and sound mind has the right to determine what shall be done with their own body (Haytand). The consent signed by the patient or his authorized representative/legal guardian upon admission is for the diagnosis and treatment. There are six essential elements in a valid consent:
- The diagnosis and explanation of the condition.
- A fair explanation of the procedures to be done and used, benefits and their potential and foreseeable consequences.
- A description of alternative treatments or procedures.
- Material rights (rights received from signing the consent), if any.
- Prognosis if ever the procedure is refused.
Consent as Proof
Consent is a written proof of the procedure that one consented to a procedure, signifying their understanding of the procedure, its benefits, risks, and possible consequences.
Ordinarily, the patient is the one to give consent on their own behalf. however, if the patient is incompetent (not of age, mentally ill) or physically unable, and there is no emergency, consent must be taken from another who is authorized to give it in his behalf.
- Minors: consent is obtained from parents or someone standing in their (the parents’) behalf. Not necessary in cases of emancipated or married minors.
- Mentally Ill: consent is obtained from parents or legal guardians.
- Emergency Situations: no consent may be obtainable in some emergencies. In these cases, no consent is necessary. The healthcare providers provide life-saving treatment as necessary.
- Refusal: a competent individual who refuses a procedure must sign a waiver of refusal against medical advice (AMA).
- Consent for Sterilization requires both the husband and wife’s permission.
Criminal Liabilities and Legal Responsibilities
Once nurses begin their practice, they become liable for their assumed authority, responsibility, and accountability in professional practice. They can be subject to scrutiny by the law and the board of nursing to ensure public welfare. Additionally, nurses can serve as expert witnesses for both plaintiffs and practitioner in a medicolegal case. For these reasons, it is necessary for professional nurses to obtain a basic understanding of the legal aspects of nursing.
A standard is the level of performance or quality against which actual practice is compared. It is the benchmark against which care is planned and implemented. Failure to deliver care up to standards can take various forms:
- Torts: intentional wrongdoing; a legal wrong that a nurse may be held accountable for in civil action. Some common examples of torts include:
- Assault: imminent threat of a harmful or offensive bodily contact, even if only verbal.
- Battery: intentional, unconsented touching of another person.
- False Imprisonment or Illegal Detection: unjustifiable detention of a person without a legal warrant or medical reason.
- Invasion of Right to Privacy and Breach of Confidentiality: the right to be left alone, free of unwanted publicity and exposure. Specifically, privacy refers to the person or identity, while confidentiality refers to data or information about an individual.
- Defamation: “character assassination”, be it written or spoken. Specifically, slander is oral defamation, and libel is written defamation.
- Negligence: the failure to fulfill (omission) a part of one’s due responsibilities in a situation where a reasonable prudent person would be able to fulfill, which results in an injury to another person or their property.
- Malpractice: the improper or unskillful care of a patient, or stepping beyond one’s authority with serious consequences.
- Incompetence: a lack of ability or legal qualification to be fit to discharge required duties. This is a ground for revocation and suspension of the certificate of registration. The nature of crime is further discussed later in this page.
Nurses, nurse trainees, and nurse volunteers are expected to be accountable for their practice, and should exercise utmost caution, critical thinking, and independent judgement to prevent incurring liabilities. Nursing aides must be supervised and limited in scope of responsibility as delegated by the nurse.
Nursing students are not permitted to perform professional nursing duties. They must be supervised, and are only given assignments at their level of training experience and competency. Guidance, orientation, and assessment is required to minimize errors.
Negligence
The failure to fulfill (omission) a part of one’s due responsibilities in a situation where a reasonable prudent person would be able to fulfill, which results in an injury to another person or their property. In a case of negligence, the actions of the person being charged is compared with set standards for care to determine whether or not negligence was present.
- Professional negligence must involve the existence of a duty, failure to meet the standard of due care, the foreseeable nature of the harm done, and injury to the plaintiff.
Legal Bases
- Civil Code, Article 19: one shall act with justice, give every man his due, observe honesty and good faith.
- Civil Code, Article 20: those who, in the performance of their obligations through negligence cause any injury to another, are liable for damages.
Negligence requires three conditions before being charged against a practitioner:
- The injury was of such nature that it would not normally occur unless negligence was present.
- The injury was caused by an agency within control of the practitioner.
- The plaintiff themself did not engage in any manner that would tend to bring about the injury (this would be a different charge).
One may defend themselves from negligence through proper documentation of care that attains the standard of care, and if the patient is a causative factor in their injury.
Doctrines in Legal Proceedings
- Doctrine of Res Ipsa Loquitur: meaning “the thing speaks for itself”, it is an action that implicitly details its consequence; no further proof is required. For example, an incident where forceps are left within the abdominal cavity after a surgical procedure speaks for itself. The forceps would not have gotten there without negligence.
- Doctrine of Force Majeure: a “superior force” that is unforeseen or inevitable. No person is responsible for these events. For example, floods, fires, earthquakes, and accidents fall under this doctrine; nurses who fail to render service during these periods are not considered negligent.
- Doctrine of Respondeat Superior: “the master must answer”. It is a doctrine dictating that the employer is responsible for the actions of their employee during their employment. For example, the hospital will be held liable if, in an effort to reduce costs, the hospital hires underboard nurses (those who have not passed the board exam) resulting in negligence from incompetence.
Other Bases for Legal Responsibilities
- The Ethical Principle of Advocacy is to participate in helping others grow and self-actualize by informing them of their rights and ascertaining that they have the right information on which to base their decisions.
- R.A. 6675, the Generics Act of 1988 specifies the requirements for valid prescriptions:
- Drugs must be written with their generic names, then brand name, or just the generic name, but never brand name alone.
- Orders are legal if they are in writing and bears the doctor’s signature. Valid orders impose a legal obligation for the nurse to follow them.
- Nurses must withhold an order if they are reasonably certain it will result in harm to the patient. In such a case, clarification with the prescribing physician is required.
- R.A. 5921, the Philippine Pharmacy Act issues provisions for pharmaceutical products, such as in pharmacist education and qualification, pharmaceutical practice, etc. Most importantly, it outlines the necessitated contents of a prescription:
- Name of the prescriber, date of prescription, their office address, professional registration number, and professional tax receipt number.
- Patient’s name, age, and sex
- Philippine Nursing Act of 1991, Section 28: IV injections require special training according to protocol established; the administration of IV injections without special training may be held liable, criminally and/or administratively. The scope of nursing duties in IV therapy include:
- Interpreting the doctor’s orders for IV therapy.
- Performance of venipuncture, insertion of needles, and cannulas except for TPN and cut down procedures.
- Preparation, administration, monitoring, and termination of intravenous solutions such as additives, intravenous medications, and intravenous push.
- Administration of blood or blood products as ordered.
- Recognition of solution and medicine incompatibilities.
- Maintenance and replacement of sites, tubing, and dressings in accordance with procedure.
- Establishment of the flowrate of solutions, medicines, blood and blood components.
- Utilization of competency in the use, care, maintenance, and evaluation of intravenous equipment.
- Nursing management of TPN and outpatient intravenous care.
- Maintenance of established infection control and aseptic nursing interventions.
- Maintenance of appropriate documentation.
- Medical Records are expected to contain full, accurate, legible, and prompt observations by nurses from the time of admission to discharge. A core principle for medical records is privacy and confidentiality.
- In times necessary, medical records can serve as legal protection for the practitioner by reflecting the disease or condition of the patient and the applied management. A common saying goes: “If it was not charted, it was not done.”
Criminal Liability
Criminal Liability is incurred if a nurse commits a felony or performs an act which would be an offense against person or property. Ignorance of the law is not an excuse for failure to comply therewith.
Crime is an act committed or omitted in violation of the law, consisting of (a) the criminal act itself and (b) evil or criminal intent. A conspiracy to commit a crime occurs when two or more persons agree to commit a crime and decide to do it. These people can be classified as:
- Principal: the “mastermind”; a member directly partaking in the crime and inducing or forcing others to aid in committing the crime.
- Accomplices: those who cooperate and are directly involved in the crime with knowledge of the malicious intentions of the act.
- Accessories: those taking part in the subsequent outcomes of the crime, e.g., profiting from stolen goods or assisting the offenders in profiting from the effects of the crime.
The Criminal Act can also be classified according to their nature and severity. Generally, there are:
- Misdemeanors: criminal offenses which do not, in law, amount to a felony. Punishment often results in fines or imprisonment in terms of less than one year.
- Felonies: a public offense for which a convicted person is liable to be sentenced to death or to be imprisoned in a penitentiary or prison. These involve deceit (deliberate intent) and fault (wrongful acts).
- Grave Felonies: those felonies to which the law attaches capital punishment (death) or penalties which in any of their periods are afflictive of imprisonment ranging from 6 years and 1 day to life imprisonment or a fine exceeding ₱6,000.00.
- Less Grave Felonies: those felonies to which the law attaches penalties of imprisonment with a maximum period of 1 month and 1 day to 6 years, or a fine not exceeding ₱6,000.00.
- Light Felonies: those infractions of law for the commission of which the penalty of arresto menor (one day to thirty days) or a fine not exceeding ₱200.00. Furthermore, these felonies are only punishable only when they have been consummated, with the exception of those felonies committed against a person or property.
- Reckless Imprudence: a type of criminal negligence where the material damage immediately results from the commission or omission of an act by the person.
- Simple Imprudence: a type of criminal negligence where the material damage is not immediately manifested or evident after the failure of a person to exercise caution and diligence in carrying out care.
The criminal act may also be classified based on the degree of execution:
- Consummated: all the necessary elements for execution and accomplishment are present.
- Frustrated: all acts to produce the felony has been performed, yet the intended result did not come about due to reasons independent of the will of the perpetrator.
- Attempted: the offender commences the criminal act, but due to unforeseen circumstances there was no complete execution to produce the desired felony.
Criminal Intent is the state of mind of a person at the time of the criminal act. It involves both freedom and intelligence, without which the act would not be a crime. In the evidence of insanity, necessity, compulsion, accident, or infancy (minors), the court decides guilt of the criminal offense.
There are, however, circumstances which can increase, reduce or completely exempt an individual from criminal liability. These are:
| Circumstances | Examples |
|---|---|
| Justifying Circumstances | Self-defense, defense for relatives, defense for strangers, defense from foreseeable threat, or the fulfillment of a duty or lawful exercise of right or office (e.g., a police officer shooting an armed drug addict |
| Exempting Circumstances | Imbeciles, insane persons (except when lucid), minors (<9), minors (>9, <15) acting without discernment, accidents, force majeure, acting from fear, or those prevented by some lawful or insuperable cau |
| Mitigating Circumstances | These do not remove liability, but rather lessens it. When the severity of wrongdoing was unforeseeable, but the initial action was intentional; <18 and >70 years of age; with sufficient threat or provocation from the offended party; in defense of relatives; if surrendered voluntarily; if with social impairment (deaf, dumb, blind, etc.) or illness that diminishes the exercise of willpower. |
| Aggravating Circumstances | These increase liability. Taking advantage of public positions, crimes committed in places of worship, crimes with evident premeditation or after an unlawful entry, crimes of abuse or confidence or obvious ungratefulness, crimes incentivized by a reward, crime committed during calamities or misfortune (theft during an epidemic), crimes involving misrepresentation (craft, fraud, disguise), and crimes supplemented by other wrongs not necessary for its commission. |
| Alternative Circumstances | Those circumstances which can be mitigating or aggravating depending on the case scenario. For example, intoxication can be mitigating if the crime was done while intoxicated; habitual intoxication, however, can be an aggravating circumstance. |
Other Crimes in Healthcare
- Moral Turpitude: act of baseness, vileness, or depravity in social or public duties, contrary to accepted and customary rights and duties between individuals.
- Murder: the unlawful killing of a human being with the intent to kill, such as in euthanasia and abortion.
- Homicide: the unlawful killing of a human being by another, given the victim is a person other than their father, mother, child, ascendants, descendants, or spouse.
- Abortion: the expulsion of products of conception before the age of viability. Procuring abortion is the charge against any individual who knowingly aids in this process.
- Infanticide: killing of a child less than three days of age. Imprisonment ranges from 2 years 4 months and 1 day, to 6 years.
- Parricide: the homicide or murder of family members whether legitimate or illegitimate. Imprisonment is for life (reclusión perpetua) to death.
- Simulation of Birth: one who enters in a birth certificate a birth that did not occur. This is a crime against the civil status of a person.
- Substitution of One Child for Another: substituting, concealing, or abandoning any legitimate child. Punishable by birth, prison mayor, and a fine not exceeding ₱1,000.00.
Avoiding Criminal Liability
(Just directly copied this one, it’s a good list.)
- Be very familiar with the Philippine nursing law.
- Beware of laws that affecting nursing practice.
- At the start of employment, get a copy of your job description, the agency’s rules, regulations and policies.
- Upgrade your skills and competence
- Accept only such responsibility that is within the scope of your employment and your job description.
- Do not delegate your responsibilities to others.
- Determine whether your subordinates are competent in the work you are assigning them.
- Develop good interpersonal relationships with your co-workers, whether they be your supervisors, peers or subordinates.
- Consult your superior for problems that may be too big for you to handle.
- Verify orders that are not clear to you or those that seem to be erroneous.
- The doctors should be informed about the patient’s conditions.
- Keep in mind the values and necessity of keeping accurate and adequate records.
- Patients are entitled to an informed consent.
Organizational Communication
Communication impacts every single management activity, and cuts all phases of the management process. The nurse-leader communicates with clients, colleagues, subordinates, and superiors. The practice of nursing often becomes group-oriented, necessitating effective interpersonal communication for continuity and productivity.
Models & Theories of Communication
| Model | Principle |
|---|---|
| Transmission Model | By Ellis and McClintock. It describes communication as a linear, one-way process in which a sender intentionally transmits a message to a receiver. There is no on-going process, simply an end point. |
| Interaction Model | By Schramm. It describes communication as an interactive, two-way process in which participants alternate positions as sender and receiver, and generate meaning by sending messages and receiving feedback. |
| Transactional Model | This extends the role of communication from an exchange of messages to a way to create relationships, alliances, self-concepts, and engage with others to create communities. Participants are called “communicators” and are simultaneously senders and receivers. |
| Interpersonal Relations | By Hildegard Peplau. She specifies the nursing communication as an interpersonal, therapeutic process that takes place when professionals engage in therapeutic relationships with people who are in need of health services. |
Peplau’s Theory of Interpersonal Relations outlines four phases of the nurse-patient relationship that the nurse must pass through for success:
- Orientation Phase: the problem is defined via assessment. The patient seeks assistance, expresses their needs, asks questions, and shares their preconceptions and expectations based on past experiences.
- Identification Phase: the patient begins to feel involved, as appropriate assistance is provided by a professional. Confidence in resolving the problem is increased. A nursing care plan is formulated in this phase.
- Exploitation Phase: professional assistance is used to determine problem-solving alternatives. The nurse uses interview techniques to explore, understand, and adequately deal with the underlying problem. This phase is the implementation phase of the nursing care plan.
- Resolution Phase: the termination of the professional relationship once the needs have been met through the nurse-patient collaboration. This phase is the evaluation phase of the nursing process.
Barriers to Communication
According to Schwarts, Lowe, and Sinclair (2010), many challenges impede communication in the healthcare setting:
- Low Health Literacy: lacking competence in acquiring and using healthcare information limits self-care for chronic conditions and medication regimens. These people are frequently dependent on facilities and have higher mortality rates.
- Cultural Diversity: communication is affected by culture— in how the content is conveyed, emphasized, and understood.
- Cultural Competence: healthcare professionals need to recognize and relate how culture is reflected in each other and in the individuals with whom they interfere.
- Interprofessional Communication Education of Healthcare Providers: communicating with other disciplines can be difficult. Jargon is varied, and the understanding or meaning of situations may be altered or incomplete.
Written Communication
Written communication is the most commonly used form of communication due to its easy distribution and nature as a document.
- Memos: used by managers for daily work life. They bring attention to problems, and they solve problems. These are not used for sensitive information, and are sent to small or moderate number of people.
- Business memos contain a header (⅛ of the paper), opening (context, task; ¼ of the paper), summary & discussion (½ of the paper), and a closing segment with necessary attachments (⅛ of the paper).
- Messages should be kept succinct. Use bullet points if possible. Keep it one page in length. The first paragraph expresses purpose— the introduction. The last paragraph is a conclusion, summarizing the memo, clarifying intended results, and main information.
- Meeting Minutes: notes or records (often by the secretary) of meetings. These include issues, motions, and votes taken, among others. These are used for those who could not attend a corporate meeting. In a normally structured meeting, these are basic steps in taking meeting minutes:
- Plan and outline. Meet with the person holding the meeting before it begins to decide on an agenda.
- Record-taking at the meeting involves the following, for each agenda of the meeting: decision made, actions (to be) taken, succeeding steps to take, voting outcomes, rejected motions, items to be held over, new business, date and time of next meeting.
- Writing the detailed notes into meeting minutes: opening (title, location, time, date), present members, absent members, approval of the agenda, approval of the previous minutes, business from previous meetings, new business, additions to the agenda, agenda for the next meeting, and adjournment.
- Submission to and approval by the chairperson.
- Distribution of meeting minutes, often as a responsibility of the secretary.
Meetings
Meetings can become effective if managed properly, with the following steps undertaken (Cherry & Jacobs, 2014):
- Pre-meeting Work: determine the purposes of the meeting. A list of meeting topics is made, and a fact sheet is created in relation to each topic. This is distributed to those in attendance.
- Determine those who will attend the meeting— those affected by decisions made during the meeting and those who may provide valuable insight for the topics.
- Schedule the meeting by date, time, and location, then invite the attendees. Consultation with the attendees will allow for maximized attendance.
- Meeting agendas (containing the aforementioned information) are distributed at least one week before the meeting, with a reminder two days before the meeting.
- During the Meeting: ensure that the participants are comfortable. In the group, there should be a leader (chairperson), timekeeper, and recorder. The leader processes one agenda at a time, allowing the timekeeper to do their job to keep the meeting on track. At the end of the meeting, debriefing is done, asking “what went well?” and “what could have been better?“. This improves subsequent meetings over time.
Reports in Nursing
Nursing reports are oral, taped, or written exchanges of information between nurses and members of the health team, such as in change-of-shift reports (endorsement), telephone orders, and transfer reports.
- Change-of-Shift Reports: the transfer of essential information and holistic care of patients, providing continuity of patient care for 24 hours. This may be done orally, by audio recording, or at the bedside during nursing rounds. Initially, oral reporting is done at the nurse’s station or conference room with nurses from the departing and arriving shifts.
- Oral Report: essential information such as patient name, diagnoses (medical, nursing), related causes, diagnostic measures completed and to be done, observations, effects of nursing and medical measures, priorities, and instructions for procedures to be done are transferred during a pre-conference. Any alarming information should be discussed out of hearing of the family.
- Audio-tape Report: outgoing nurses relay recordings of pertinent information. The lack of immediate feedback on inquiries is a major disadvantage of this method.
- Nursing Rounds: endorsement at bedside, where the care plan is discussed, allowing the patient and family to participate, pose questions, and seek clarifications. Any additional assessments and evaluations can also be made at this time.
- Telephone Reports: physicians or other nurses may be updated about patients via telephone. All information transmitted should be transcribed accurately, especially if medications are involved or if significant variances have occurred. The date, time, name of the physician, and signature of the nurse receiving telephone orders are all documented to be countersigned within 24 hours.
- Transfer Reports: patients being transferred from one unit to another require proper referral and coordination. The receiving unit is usually advised beforehand about the transfer so that the unit or bed including special equipment, if necessary, will be arranged. All pertinent information for the continuity of care is provided to the receiving unit, including a summary of medical progress and current health status. An oral report is also made by the accompanying nurse so that additional information can be made or clarified. A transfer report accompanies the patient.
Patient Satisfaction & Customer Service
Nurses need to provide a comprehensive range of patient needs. In settings where facilities desire for patients to use their services, nurses are expected to keep patient satisfaction and customer service, which includes safety and quality care as the leading motivator of all plans and activities (Cherry & Jacobs, 2014). Customers may be categorized as external or internal:
- External customers: those not employed by the organization (patients, families, referral physicians, payers e.g. insurance companies, managed care plans).
- Internal customers: those employed by the organization (patient care staff members, staff members of departments, administrators, social workers, dietitians, therapists, etc.)