Unconscious patients are among the most ethically and legally concerning cases. Consciousness is the state of awareness of oneself and their surroundings. It is the ability to perceive sensory stimuli and respond appropriately to them. Its abnormal state— non-arousability and unresponsiveness at its most severe state, is a coma. It is a symptom, rather than a disease by itself. It varies in profoundness and duration, ranging from fainting to a deep coma.
- Unaware of surroundings and does not respond to sound, questions, and touch
- Makes no purposeful movements, loss of bowel or bladder continence
- Confused, drowsy
- Respiratory function changes
- Abnormal pupil reactions
Patients recovering from altered level of consciousness or even deep comas vary, with some recovering with no long term residual effects, some with residual damage (learning deficits, emotional difficulties, impaired judgment). Some may remain in a persistent vegetative state (cerebral/brain death).
Diagnostic Tests
- Imaging:
- X-ray
- Magnetic Resonance Imaging (MRI): for clearer images of soft tissues; tumors, vascular abnormalities, and intracranial bleeding.
- Computerized Tomography (CT): imaging of soft tissues, bones, fat, and organs.
- Lumbar Puncture (LP): analysis of cerebrospinal fluid; cerebral meningitis, CSF evalution
- Positron Emission Tomography (PET)
- Electroencephalogram (EEG)
- Blood Testing: CBC, LFT, RFT, ABGs, etc.
Medical Management
The goal of medical management in unconscious patients is to preserve brain function and prevent further damage. This invovles:
- Ventilator Support and Oxygen Therapy for those with altered respiratory function.
- Blood pressure management
- Fluid balance management
- Seizure management: the use of antiepileptics, sedatives, and paralytic agents.
Increased Intracranial Pressure (ICP)
- Mannitol (diuretic) and corticosteriods that reduce intracranial pressure.
- Management of temperature regulation: ice packs, tepid sponge bath (TSB), antipyretics, NSAIDs
- Management of elimination: laxatives, high-fiber diet (avoid constipation → straining → increased ICP)
- Management of nutrition: TPN and RT (Ryle’s Tube) feeding
- Deep Vein Thrombosis Prophylaxis
- Craniotomy with subcutaneous bone flat storage
- Cranioplasty
- Burr-hole
Nursing Management
- Maintain adequate cerebral perfusion.
- Remain normothermic.
- Be free from pain, discomfort, and infection.
- Attain maximal cognitive, motor, and sensory function.
Glasgow Coma Scale (GCS)
Glasgow Coma Scale
A three-category test to score a patient’s mental functioning out of 15 (lowest being 3). A score of 13 to 15 may only show for minor/mild brain injuries (15 indicates good orientation), 9 to 12 for moderate brain injuries, and 3 to 8 for severe brain injuries (3 indicates deep coma).
| Criteria and Scoring | ||
|---|---|---|
| Response | Scale | Score |
| Eye Opening Response | Eyes open spontaneously | 4 |
| Eyes open to verbal command, speech, or shout | 3 | |
| Eyes open to pain (not applied to face) | 2 | |
| No eye opening | 1 | |
| Verbal Response | Oriented | 5 |
| Confused conversation, but able to answer questions | 4 | |
| Inappropriate responses, words discernible | 3 | |
| Incomprehensible sounds or speech | 2 | |
| No verbal response | 1 | |
| Motor Response | Obeys commands for movement | 6 |
| Purposeful movement to painful stimulus | 5 | |
| Withdraws from pain | 4 | |
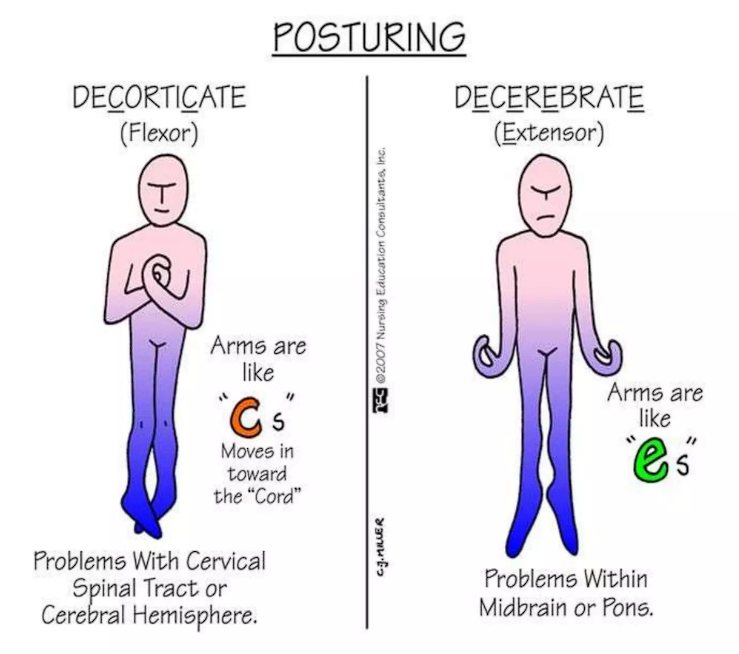
| Abnormal (spastic) flexion, decorticate posture | 3 | |
| Extensor (rigid) response, decerebrate posture | 2 | |
| No motor response | 1 | |
| Category | Description |
|---|---|
| Alert/Full Consciousness | Responds immediately to minimal external (visual, tactile, auditory) stimuli |
| Lethargic | A state of drowsiness; the client needs increased external stimuli to be awakened but remains easily aroused. Verbal, mental, and motor responses are slow or sluggish. |
| Obtunded | Very drowsy when not stimulated, but is able to follow simple commands when stimulated vigorously (shaken, shouting). Verbal responses are simple (few words) and the client will drift back to sleep between periods of stimulation. |
| Stuporous | Awakens only to vigorous and continuous noxious (painful) stimulation. There is minimal spontaneous movement; motor response to pain is normal but verbal responses are minimal and often incomprehensible (moaning, groaning) |
| Light Coma | Vigorous stimulation does not produce a response. Only motor responses to noxious stimuli are still purposeful. |
| Deep Coma | Same as light coma, but Motor responses to noxious stimuli are absent. |
Limitations to the descriptive nature of a GCS can arise from:
- Eye Opening: if severe facial/eye swelling/ptosis is present, eye responses may be inaccurate or unmeasurable. Some patients with flaccid eye muscles can also keep their eyes open if drawn back, while being very different from spontaneous eye opening. This is still recorded as a score of zero.
- Verbal Response: patients on endotracheal/tracheostomy tube or patients with hearing defects or speech defects will have altered responses. Written instructions may be used.
- Motor Response: asymmetrical responses (focal deficit) may be observed. If this is the case, the stronger response is recorded, e.g., if a patient is able to localize pain on the left side, but flexes to pain on the right side, the former is recorded.
Physical Assessment
- Voluntary Movement: strength and asymmetry in the upper extremities
- Deep tendon Reflexes: biceps, triceps, and patella
- Pupillary Light Reflex: pupil size
- Corneal Blink Reflex
- Gag Swallowing Reflex
- Posturing: decorticate and decerebrate postures
Potential Nursing Diagnoses
- Ineffective airway clearance
- Ineffective cerebral tissue perfusion
- Risk for increased ICP
- Imbalanced fluid volume
- Impaired skin integrity
- Self-care deficit
- Imbalanced nutrition
- Incontinence: bowel and/or bladder
- Risk for aspiration
- Risk for contractures
- Altered family process
Airway Maintenance
- Breath sounds are assessed every two hours.
- ABG testing is done regularly to determine oxygenation.
- Assess for cough and swallow reflexes.
- An artificial airway may be used; tracheostomy or endotracheal intubation and mechanical ventilation may be necessary.
- Avoid obstructions:
- Position the client on alternate sides every two to four hours to prevent the accumulation of secretions on one side.
- Maintain the neck in a neutral position.
- Oronasopharyngeal suctioning may be done as necessary.
- If facial palsy or hemiparalysis is present, keep the affected side up/the uppermost.
- Chest physiotherapy and postural drainage may be done to assist in the removal of tenacious secretions.
- Remove dentures
- Oral care is given to avoid upper respiratory tract infection.
Cerebral Tissue Perfusion and Increased ICP
- Monitor GCS, SpO₂, ABGs, and vital signs (particularly increased temperature).
- High temperature can be corrected with antipyretics and cooling measures.
- Position the head at an elevation of 30° maintained to facilitate venous drainage, along with a neutral position.
- Reduce agitation (utilize sedation if necessary).
- Reduce cerebral edema. The drug of choice for cerebral edema is Mannitol, an osmotic diuretic. Loop diuretics and corticosteroids also reduce cerebral edema. Edema caused by trauma generally peaks within 72 hours post-trauma and subsides gradually.
- Mannitol 20 to 50 grams IV bolus is given if ICP exceeds 20 mmHg, as prescribed.
- Harsh activities (suctioning, bathing, turning) are spaced apart to give breaks for recovery.
- Minimize stimulation; speak softly and limit touch.
- Administer laxatives, antitussives, and antiemetics as ordered. Constipation, coughing, and vomiting all increase intracranial pressure and can contribute to decreased perfusion.
- Prevent seizures with antiepileptics (Dilantin) as ordered.
Monitor for signs of rising ICP, such as restlessness, headaches, pupillary changes (assessed hourly), respiratory irregularity, and Cushing’s triad (widening pulse pressure, hypertension, bradycardia). Remember the normal ICP must stay within 5 to 15 mm Hg.
Imbalanced Fluid and Electrolyte
The main method of monitoring F&E is with a meticulously maintained intake-output chart. The daily weight of the patient should be recorded to determine fluid retention. 1 L of fluid retained will translate to 1 kg of body weight. Any symptoms that may indicate fluid volume overload or deficit should be assessed and documented.
- Diuretics may be prescribed to correct fluid overload and reduce enema.
- Overhydration and IVF with glucose are always avoided in comatose patients, as these may result in cerebral edema.
Impaired Skin Integrity
The nurse provides interventions for all self-care needs if the patient is unable to do so for themselves. This includes bathing, hair care, skin care, and nail care (trimming). Frequent back care should be given as it is a primary area of discomfort in immobile patients.
- Comfort devices should be used; special mattresses or airbeds are used.
- Positioning should be changed regularly.
- Adequate nutritional and hydration status should be maintained.
- The eyes should also be kept moist by instilling methylcellulose. Protective eye shields can be used, or the eyelids can be closed with adhesive strips if corneal reflex is absent. These avoid corneal abrasions and irritation.
- Inspect the oral cavity. Oral hygiene is given every 4 hours. Keep the lips coated with a water-soluble lubricant to prevent encrustation, drying, and cracking. Paralyzed cheeks are inspected. The nasal passages may also become occluded. They may be cleaned with a cotton-tipped applicator.
- Positioning is imperative. The position should be alternated between sides every two to four hours. If the patient is hemiplegic, the affected side is only used for brief periods.
- Lateral position on a pillow: neutral head position
- Upper arm positioned on a pillow: shoulder alignment
- Upper leg supported on a pillow: hip alignment
Self-Care Deficit
Attending to the hygiene needs of the unconscious patient should never become ritualistic. Dignity is maintained at all times. Hygiene is a major contributor to pressure ulcers, along with incontinence, perspiration, poor nutrition, obesity, and old age. The skin is properly examined, noting any dry, red, or broken areas.
- Bathing: two nurses bathe an unconscious patient. Make to prevent airway obstruction. Include proper hair care and assess the skin when giving a bed bath.
- Oral Hygiene: a chlorhexidine-based solution is used for oral care. Maintaining oral cleanliness (at least every four hours) reduces the risk of infection. Airways, if possible, are removed, cleaned, and reinserted. If an ETT is in place, the tube should be fixed alternately on each side. Take care to not damage the gums with excessive force.
- Eye Care: observe for irritation, abrasion, corneal drying, and edema. The eyes are gently cleaned with gauze and 0.9% sodium chloride to prevent infection. Artificial tears can also be applied as drops to help moisten the eyes. If the eyes remain open for a long time, corneal damage can occur; the use of adhesive strips can aid in closing the eyes.
- Nasal Care: nasal mucosa may be cleaned with gauze and water. An NGT can damage the nasal mucosa, so pressure spots are inspected and the side used is alternated.
- Ear Care: the surroundings of the aural canal should be cleaned. Take care not to push anything into the ear canal.
Imbalanced Nutrition
Diet is prescribed based on the individual’s requirements specifically to meet energy needs, aid in tissue repair, replace fluid loss, all to maintain basic life functions. This may be done via:
- TPN for prolonged unconsciousness.
- Enteral Feeding via NGT, NJT, or PEG tube.
Risk for Injury
A cardinal rule is to keep side rails up when the patient is not receiving direct care. Seizure precautions must be taken. Other causes of injury include:
- Moving and turning: make sure to provide adequate support to the limbs and head. Protect the patient from external sources of heat.
- Oversedation can impede LOC assessment and causes respiratory depression.
- Restraints are not used unless highly necessary. Restraints are also regularly released (every 2 hours).
Impaired Elimination Functions
Assess the patient for constipation and bladder distention:
- Bowel sounds should be auscultated. If necessary, stool softeners or laxatives may be igiven.
- Bladder Catheterization may be done if ordered. Catheter care is provided with aseptic technique to prevent CAUTIs. The urine output and color is monitored. Bladder training is started as soon as the patient regains consciousness in order to remove the need of a catheter, which is a source of infection.
Risk for Contractures
Contractures can form in immobile patients. Maintain the extremities in functional positions by providing proper support. Support devices should be removed every four hours to allow for passive exercises and skin care. Foot support should be provided.
Altered Family Process
The family members should be included in the patient’s care. Communicate frequently with them, and allow them to stay with the patient when possible. Aid the family in using external support systems (counsellors, religious clergy, etc.) and provide any information or clarifications they may require. Encourage them to share their inquiries and concerns.
Sensory Stimulation
The brain needs sensory inputs to maintain activity, as if exercising. In patients, the sense of hearing is often the last to be lost, whether in unconsciousness, coma, or death. The patient should always be communicated with when procedures are being performed, despite the appearance of unconsciousness. Many clients remember audible events or dialogue while they were “sleeping”, and some report longing for someone to communicate with them. The nurses should always show respect and maintain privacy. The family is encouraged to contribute to the care of their loved ones.