The following discussion is the complete summary of the following notes, based on the 2nd edition of Dr. Rosalinda Parado Salustiano’s Maternal and Newborn Care: A Comprehensive Review Guide textbook, and the discussions of Sir Francis Vasquez.
These are the fragmented notes combined into this page:
- 02-18-2024 Normal OB (Fertilization, Fetal Development, Discomforts)
- 05-05-2024 Normal OB (Family Planning and Induction/Augmentation of Labor)
- 08-27-2024 Normal OB (Anatomy)
- 09-09-2024 Normal OB (Prenatal Checkup, Estimates of Pregnancy, Pelvic Exam)
- 09-10-2024 Normal OB (Labor and Delivery)
- Chapter 01: The Male Reproductive System
- Chapter 02: The Female Reproductive System
- Chapter 03: The Menstrual Cycle
- Chapter 04: Fertilization and Fetal Development
- Chapter 05: The Antepartal Period
- Chapter 07: The Intrapartal Period
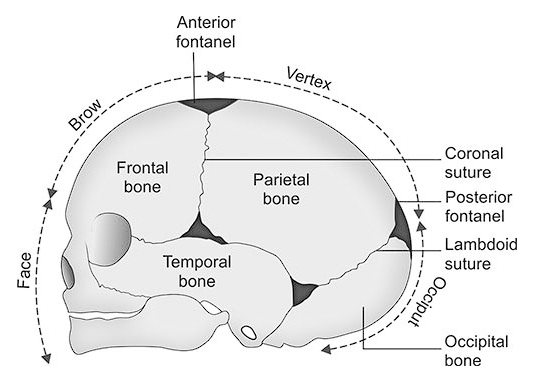
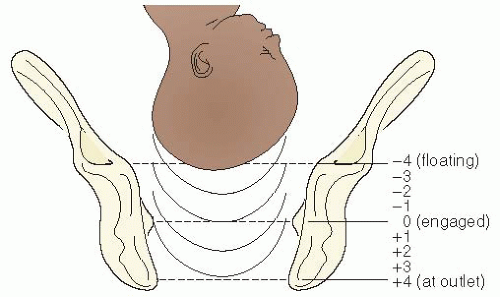
- Chapter 08: The Fetus During Labor
Enjoy the read.
Pregnancies must be planned, wanted, and supported; adequately managed/monitored; facility-based; and secures proper postpartum and newborn and childhood care (MNCHN, DOH, Administrative Order 2008-0029: Implementing Health Reforms for the Rapid Reduction of Maternal and Neonatal Mortality).
- Planned: the mother takes into consideration the desired number of children, adequate child spacing (at least three to five years, five years for C.S.), and proper timing with appropriate pre-pregnant parameters (age, weight).
- Timing may be during average maternal age (18 to 35), and after the attainment of acceptable weight (90 to 150 lbs.), etc.
- The recommended number of children is 2 to 3. Each birth is followed by an interval of 3 to 5 years; 5 years for C.S. children.
- Monitored: a facility-based prenatal checkup by trained and professional staff. An adequate number of frequency of prenatal visits should be met, more frequent if indicated.
| Trimester | DOH (4 total visits) | WHO (14 total visits) | RPS (14 total visits) |
|---|---|---|---|
| 1st Trimester | Once before the fourth month | Once a month | Once a month |
| 2nd Trimester | Once before the sixth month | Once every two weeks | Once a month |
| 3rd Trimester | Once before the eighth month | Once a week | Once a month (to 8th month), then twice a month for the third month |
| Final Month | Once on the final month | Once | Once a week on the final month (36th to 40th week) |
Male Anatomy
Reference
Salustiano, R. (2024). The Male Reproductive System. In Dr. RPS Maternal & Newborn Care: A Comprehensive Review Guide and Source Book for Teaching and Learning (2nd ed., pp. 2-22). C&E Publishing, Inc.
Andrology is the study of the male reproductive system and urological problems. The primary reproductive function serves to produce and transport sperm through and out of the genital tract into the female genital tract. It is composed of the penis, scrotum, testes (testosterone, sperm), ducts (seminiferous tubules, epididymis, spermatic cord), accessory glands (seminal vesicles, prostate glands, Cowper’s glands, urethra).
The Penis
The penis is an elongated and cylindrical appendage, consisting of a body (shaft) and a cone-shaped end (glans). Within it is the urethra, a passageway for both urine (excretory function) and semen (reproductive function, primary). It lies in front of the scrotum. The penile root lies in the perineum, from where it passes forward below the symphysis pubis, while the lower two-thirds are outside the body in front of the scrotum and covered in skin. It is extremely vascular; blood spaces fill and become distended during sexual excitement, resulting in penile distention and stiffening, termed as an erection. The erectile tissue is composed of three columns, of two types:
- Corpora Cavernosa (two columns): lateral columns located on either side and in front of the urethra
- Corpus Spongiosum (one column): posterior column, which contains the urethra. The tip is expanded to form the glans penis. The skin at the end of the penis is folded back on itself above the glans penis to form the prepuce (foreskin), a movable double fold.
Stimulation of the parasympathetic system causes contraction of the ischiocavernous muscle, which prevents the return of venous blood from the cavernous sinuses. The blood vessels engorge, and the penis becomes elongated, thickened, and stiff. If stimulation is intense, there is rhythmic contraction of the penile muscles, resulting in the forceful and sudden expulsion of semen, a phenomenon called ejaculation.
- Released with ejaculation is about 2 to 4 mL (or 1.25 to 5 mL) of semen containing about 100 million sperm per mL, of which about 20% to 25% are likely abnormal; sperms move at a speed of 2 to 3 mm per minute. In a single ejaculation, the male deposits approximately 200 to 400 million spermatozoa in the vagina, of which fewer than 200 actually reach the ampulla.
- A successful sperm can fertilize an ovum in 5 to 30 minutes after ejaculation.
- Volume and force of ejaculate varies due to some factors:
- Age: males tend to ejaculate the largest volume of semen in their thirties; decreases with age.
- Sexual activity: decreased semen volume with recent sexual activity/masturbation reduces the distance semen can travel; increased semen volume than usual with prolonged periods of abstinence.
- Genetic factors: some people naturally ejaculate more or less compared to others, regardless of health or lifestyle.
- Lifestyle factors: diet, smoking, and other lifestyle factors can affect semen quality and overall health; regular exercise may improve fertility, sperm quality, and semen volume.
- Overall health: injury, chronic illness, or surgery causing nerve damage may affect semen volume and quality.
- Certain drugs: there are certain drugs that interfere with the production of sperm (anabolic drugs, testosterone, chemotherapy medication, opioids), antibiotic ketoconazole, and long-term use of antidepressant selective serotonin reuptake inhibitors (SSRIs).
Phases of Sexual Response
(mn. APOR, EPOR)
- Arousal/Excitement: the sexual stimulation by physical or mental stimuli such as touch, kissing, fantasizing, or viewing erotic images.
- Plateau: the period of increasing sexual excitement during which the penis, vagina, and clitoris will engorge with blood and become highly sensitive.
- Orgasm: the spontaneous release of sexual energy accompanied by rapid contractions of the lower pelvic muscles, including ejaculation.
- Resolution: the gradual return to the normal level of functioning and swollen or erect body parts return to their normal sizes. This phase also includes refractory period.
The Scrotum
The sac-like or pouch-like structure from the root of the penis, suspended from the perineal region. It contains the testes and epididymis, and primarily serves to maintain a lower temperature than the body (by ~1°C) to protect the testes and sperm, and promote spermatogenesis.
- Nursing Implication: when educating for testicular self-examination (TSE), the best timing for checking is after a warm bath or shower when the scrotum is soft and less wrinkled, allowing for better palpation of the testes.
- Nursing Implication: in newborns, perform assessment of successful descent of the testes (palpation of the scrotum) from the abdominal cavity. Failure to do so will result in failure for spermatogenesis to occur. This condition is known as cryptorchidism.
Testes
Two small (4.5 cm to 6 cm long, 2.5 cm wide, 3 cm thick), oval male gonads are suspended in the scrotum, weighing 10 to 15 grams. They secrete male sex hormones (androgens) and are the site of spermatozoa production in the mature male. They have endocrine and exocrine functions:
- Endocrine Function: the process of spermatogenesis and the other functions of the testes are under neural and hormonal control. Several structures contribute. Hormonal balance must be maintained in order to maintain proper development of sperm, and infertility can result from a hormonal imbalance.
- The Hypothalamus stimulate or inhibit APG secretions.
- The APG secretes the gonadotropins FSH (stimulates Sertoli cells) and LH (stimulates Leydig cells).
- The Testes are the site of testosterone production, through special Leydig cells that synthesize testosterone from cholesterol. These also locally support sperm production.
- Exocrine Function: spermatogenesis begins during puberty, where the germinal epithelium in the seminiferous tubules begin producing male gamete (sperm) under the influence of follicle-stimulating hormone and testosterone. This process continues throughout adult life.
The testes are covered into three testicular layers. They are covered by tunica vaginalis, under which is the tunica albuginea, a tough, fibrous, white capsule that covers each testis. It sends inward projections that divide the testis into 250 to 400 lobules, which each contain one to three convoluted seminiferous tubules containing sperm cells in various stages of development. An additional inner layer of connective tissue which contains a fine network of capillaries is the tunica vasculosa, the innermost of the testicular covering layers.
Sertoli cells are special cells that provide structural and metabolic support to the developing sperm cells, being in close contact with the spermatogenic cells at all stages of differentiation. They extend from the basement membrane to the lumen of the seminiferous tubule.
- Maintains the environment necessary for development and maturation.
- Secretes substances initiating meiosis.
- Secretes supporting testicular fluid.
- Secretes androgen-binding protein, which keeps testosterone close to the developing gametes.
- Secretes hormones effecting pituitary gland control of spermatogenesis, particularly the hormone inhibin.
- Phagocytose residual cytoplasm left over from spermiogenesis.
Sperm Production
The primary spermatogonia, the primitive germ cell, are present at birth with diploid 44XY cells. After puberty, spermatogenesis is continuous and is completed in 72 hours. There are various stages:
- Spermato-Cytogenesis: the diploid spermatogonium produces primary spermatocytes (44XY), which undergo meiosis into two secondary spermatocytes (now a haploid; 22X or 22Y).
- Spermatidogenesis: second meiotic cell division produces four spermatids.
- Spermiogenesis: the spermatids grow a tail, develops a mid-piece where mitochondria gather and form an axoneme, and removing residual cytoplasm and organelles to form four spermatozoa/sperms (22X or 22Y). The nucleus becomes compacted in the head of the sperm, and covered with a cap (acrosome).
- Spermination Process: occurs when mature, non-motile spermatozoa are released from protective Sertoli cells (the “nursing cells of the testes) into the lumen of the seminiferous tubules.
flowchart LR
A(Diploid Spermatogonium)
B(Primary Spermatocyte)
C(Spermatids)
D(Spermatozoa)
A-->B-->C-->D
Sperm production creates about 1,000 sperm cells every second, and maturation takes ~9 to 10 weeks for full development and maturation (~70 days in the testes, ~12 to 26 days in the epididymis). Comparatively, a woman’s egg cells are all already present at birth, and are cyclically released.
Sperm Cells
Sperm cells generally live for three to five days if released within the female reproductive tract, but dies within minutes if released into the open. If ejaculation does not occur, sperm remains within the body for ~74 days before dying and being recycled.
| Androsperm (22Y) | Gynosperm (22X) |
|---|---|
| Carries the Y chromosome | Carries the X chromosome |
| Fast-moving | Slow-moving |
| Smaller, weaker, short-lived | Bigger, stronger, long-lived |
| Acid-sensitive | Acid-resistant |
Who determines the gender of the child?
The female gamete contains XX sex chromosomes, one of which is used for the child. The other is from the male gamete, which contains XY sex chromosomes. Conception resulting in XY sex chromosomes produce males and XX produces females. From this, as the father has the determining X or Y chromosome, he determines the sex of the offspring.
Sperm anatomy is divided between the head, neck, body, and tail:
- Head: spheric shape containing a large nucleus, made up of chromosomal material compacted with all the genetic information and 23 chromosomes. Its high compression allows for the sperm to be small, light, and fast. The tip of the head is covered by a cap called an acrosome, which contain hyaluronidase enzyme that can break through the protective covering of an egg cell (zona pellucida) by destroying the hyaluronic acid of the cell during fertilization.
- Neck: contains the proximal and distal centrioles
- Body/Middle-piece: an important part containing spirally arrange mitochondria, that provides energy for the sperm.
- Tail: the flagellum, which aids in motility through the male and female reproductive system.
Testosterone
The primary male hormone. It is responsible for the regulation of sex differentiation, expression of male sex characteristics, spermatogenesis, and fertility.
- Its effects are first seen in the fetus; Gonadal development begins at 5 to 6 weeks (prior to this, reproductive tissue is identical in both genders of the fetus). Around week 7 in utero, the sex-determining region Y (SRY) from the Y chromosome initiates the development of the testicles. Development results in the beginning of the production of testosterone, and begins acting on the body throughout life.
- Secondary sexual characteristics developed by testosterone include: growth (height, muscle, bone), vocal deepening, reproductive system growth, and hair (face, chest, axilla, pubis).
- Spermatogenesis (by the seminiferous tubules) is aided by testosterone, along with FSH.
The Duct System of the Testis
- Seminiferous Tubules: the “seed-carrying” tubules. It is the site of sperm production (spermatogenesis).
- Epididymis: soft, cord-like, and comma-shaped, located on the superior surface of the testis, travelling down the posterior aspect of the lower pole of the testis, leading to the deferent duct (vas deferens).
- Spermatic Cord: contains the vas deferens, blood vessels, nerves, and lymphatic vessels. The vas deferens joins the duct of seminal vesicles to become ejaculatory ducts; small muscular ducts that carry the spermatozoa and the seminal fluid to the urethra.
Accessory Glands
- Seminal Vesicles: paired structures or pouches situated posterior to the bladder. They are 5-cm long and pyramid shaped, and contributes to the ejaculate. This provides nutrition (fructose) for the sperm. It also contains mucus and prostaglandin (causes uterine contraction to aid in sperm motility.
- Prostate Gland: just below the bladder, surrounding the urethra at the base of the bladder, and lies between the rectum and the symphysis pubis. It is 4-cm long, 3-cm wide, and 2-cm deep. It is composed of columnar epithelium, a muscular layer and enclosed in a form outer fibrous layer/capsule. It connects to the urethra and ejaculatory ducts, and secretes a thin, lubricating milky fluid that enters the urethra through the ducts and helps in the passage and viability of spermatozoa. It contributes alkaline to the sperm, which give it its scent and protects against the acidic environment of the vaginal canal.
Döderlein bacilli are responsible for acidity of the vaginal canal, as it produces lactic acid from glycogen in the lining of the vagina. This protects the vagina, but is harmful to the sperm.
- Cowper’s Glands: located on each side of the urethra, just below the prostate gland; it secretes a small amount of lubricating fluid.
- Urethra: the conduit of semen (sperm with fluids) outside the body through the penis.
| Unit | Contribution to Seminal Fluid |
|---|---|
| Epididymis | 5% |
| Seminal Vesicle | 30% |
| Prostate Gland | 60% |
| Cowper’s Gland | 5% |
flowchart LR
A(Seminiferous Tubules)
B(Epididymis)
C(Vas Deferens)
D(Seminal Vesicles)
E(Prostate)
F(Cowper's Gland)
G(Urethra)
H(Outside)
A-->B-->C-->D-->E-->F-->G-->H
Sperm Analysis
A sperm analysis is a simple, non-invasive test for assessing infertility and other potential abnormalities. Preparation requires abstinence for 2 to 3 days (at least 48 hours) prior to specimen collection. Specimen collection, as always, should be done in a clean container. The specimen is kept at body temperature and delivered to the laboratory within 30 to 45 minutes, or up to 60 minutes. Earlier is better.
Obtaining Accurate Results
The test may be repeated in 2 to 4 weeks due to variance between specimens. Because of the duration of spermatogenesis (2.5 months), 2 to 3 specimens may be obtained over several months.
Contesting reference values were found between p. 15 (Semen Analysis: Preparation/Procedure) and p. 21 (Semen Analysis Results).
| Semen Analysis Results | Normal Findings |
|---|---|
| Volume | 2 to 6 mL, with a pH of 7 to 8 |
| Viscosity | liquid within 30 minutes (or 20 minutes) |
| Sperm Count | more than 20 million/mL |
| Morphology | more than 50% are mature and normal |
| Motility | more than 40% (or 50%) are moving |
| Leucocytes | <1 million/mL |
| Semen Analysis Results | Reference Range (WHO) |
|---|---|
| Total sperm count in ejaculate | 39 to 928 million |
| Ejaculate volume | 1.5 to 7.6 mL |
| Sperm concentration | 15 to 259 million per mL |
| Total motility (progressive and non-progressive) | 40 to 81% |
| Progressive motility | 32 to 75% |
| Sperm morphology | 4 to 48% |
Other considerations for low sperm count if it is seemingly idiopathic:
- Activities that increase scrotal heat: frequent hot tub or sauna use, long period of sitting, or clothing (tight-fitting)
- Alcohol and drug use, such as marijuana
- Frequency of ejaculation
- Men whose mothers took diethylstilbestrol (DES) while pregnant
- Trauma/surgery to the testes.
Female Anatomy
Reference
Salustiano, R. (2024). The Female Reproductive System. In Dr. RPS Maternal & Newborn Care: A Comprehensive Review Guide and Source Book for Teaching and Learning (2nd ed., pp. 23-49). C&E Publishing, Inc.
The Vulva
The external genitalia of the female are collectively called the vulva. The pudenda is commonly designated the vulva.
The external soft, rounded, fatty pads that cushion over the symphysis pubis for protection is the mons veneris or mons pubis. This is the area covered by the triangular area known as the escutcheon, where curly hair grows after puberty.
The labia majora, “bigger lips”, are two folds of skin with sparse hair on either side of the vaginal opening. It contains fat and Bartholin’s glands (provides lubrication) that protects the labia minora and vaginal os. The labia minora, “smaller lips”, are two thinner folds of delicate tissue within the labia majora, usually not visible behind the non-separated labia majora in nulliparas but common to project beyond the labia majora in multiparas. It is hairless, moist, and reddish (as if a mucous membrane), and contains many sebaceous follicles and a few sweat glands.
- Each labia minora superiorly bifurcate then converge into two lamellae with each pair, the anterior or upper pair forms the prepuce, and the lower pair fuse to form the frenulum of the clitoris.
- Inferiorly, the labia minora simply converges into the fourchette. The labia minora act to protect and obscure the vestibule, urinary meatus, and vaginal os.
The clitoris is a small body of highly erectile, erogenous, and sensitive tissue protected by the prepuce. It is composed a glans, a corpus, and two crura. It measures less than 1 cm in width by 2 cm in length, with less than 0.5 cm in diameter. It is covered by stratified squamous epithelium that is richly supplied with nerve endings (more than 10,000!); the vessels of the clitoris are connected with the vestibular bulbs. As such, it is sensitive to touch, pressure, and temperature. This makes it the primary site of sexual arousal, excitement, and orgasm. The principal female erogenous organ.
- In obstetrics, the clitoris is used as a landmark to guide female catheterization.
- It is the site of syphilitic chancre (in young women) and leukoplakia (in mature women).
Bounded by the labia minora, clitoris, and fourchette, the almond-shaped area with six openings is called the vestibule. The six openings include the urethral meatus, vaginal opening, and two Skene’s glands and two Bartholin’s glands.
- Urethral Opening/Meatus: the anterior opening set midline, 1 to 1.5 cm below the pubic arch, above the vaginal os, and below the clitoris. This is how the clitoris functions as a landmark for catheterization. The urethra’s short length predisposes women to urinary tract infection.
- Vaginal Opening: the posterior opening, often hidden by overlapping labia minora in virginal women. An area called the fossa navicularis lies posterior to the vagina to the fourchette, usually only observed in nulliparous women.
- Hymen: a thin membrane of various thickness, with no glandular or muscular elements and not richly supplied with nerve fibers. It surrounds the vaginal opening, and protects it.
- Skene’s Glands or Paraurethral Glands: two small, palpable glands that open into the posterior urethral wall. They secrete mucus to lubricate the vestibule.
- Bartholin’s Glands or Vulvovaginal Glands: two small, palpable glands situated beneath the vestibule on either side of the vaginal opening. At sexual arousal, these glands secrete alkaline mucoid material, altering the vaginal canal environment to favor motility and viability of sperms, particularly of androsperms (which are weak to acid).
The perineum is the area between the vagina and the rectum, consisting of fibromuscular tissue.
Internal Female Reproductive Organs
The vagina is a vascular, tubular, and musculomembranous structure that extends from the vulva to the uterus between the urinary bladder (anteriorly) and rectum (posteriorly). Its length is 3” to 4”, with its posterior wall 10-cm long and anterior wall 7.5-cm long. It is the female organ of copulation, and the excretory canal of the uterus through which uterine secretions and menstrual flow escape. It also becomes a soft birth canal during labor.
- The vagina has rugae (folds), transverse ridges of mucous membranes lining the vagina, which allow it to stretch during sexual intercourse and childbirth.
- Vaginal pH is normally 4 to 6 pH. This acidity is created by Döderlein’s bacilli consuming glycogen in the inner lining of the vagina, and producing lactic acid as a result.
The uterus is the hollow, muscular, pear-shaped (pyriform) organ; covered partially by the peritoneum or serosa, lying between the base of the bladder anteriorly and the rectum posteriorly. It is 7.5 cm by 5 cm by 2.5 cm, with each wall being 1.25 cm thick.
- Length varies, being 2.5 cm to 3.5 cm pre-puberty, 6 cm to 8 cm in adult nulliparous women, and 9 to 10 cm in multiparous women.
- Weight is ~60 grams while nonpregnant, to ~1,000 grams in pregnancy.
- The uterine walls consists of three layers:
- Endometrium: the inner mucosal layer; undergoes constant changes in response to estrogen (during the proliferative phase), and progesterone (during the secretory phase) in the menstrual cycle. It becomes highly specialized and is called the decidua during pregnancy.
- Myometrium: the middle muscular layer; the living ligatures that control bleeding during the third stage of labor. This responds to stimulation by oxytocic drugs.
- Perimetrium: the outer serosal layer formed by the peritoneum; continuous with broad ligaments on the sides of the uterus.
Various parts and regions make up the uterus:
- Fundus: convex upper part between the insertion of the fallopian tubes; the most contractile portion of the uterus during labor.
- Corpus or body: the upper, larger, triangular portion of the uterus.
- Cornua: the portion or point from where the oviducts or the fallopian tubes emerge.
- Isthmus: constricted area immediately above the cervix: the lower uterine segment; distends during pregnancy.
- Cervix: the lower, smaller cylindrical portion with an internal os, the cervical canal, and an external os.
The uterus is partially mobile. It is free to move along the anteroposterior plane as the body moves. Normally, the uterus is almost horizontal when a nonpregnant woman stands erect. Depending on its position, it can be characterized as:
- Anteversion: leaning forward
- Anteflexion: bending forward on itself, with the fundus resting on the bladder. With anteversion, these positions prevent uterine prolapse.
- Retroflexion: an abnormal position where the uterus bends back towards the cervix, resulting in a sharp angle at the point of bending.
- Retroversion: turning back of the entire uterus in relation to the pelvic area.
The movement of the uterus is limited and supported by the pelvic floor and several ligaments, the most important of which are at the level of the cervix.
- Broad Ligament: extends from the lateral margins of the uterus to the pelvic walls, thereby dividing the pelvic cavity into the anterior and posterior compartments. The lower border is thickened and strengthened to form the most important uterine support—the transverse cervical ligament—which, when damaged during labor, may cause the uterus to sag downward.
- Round Ligaments: arises from the cornua of the uterus in front and below the insertion of each uterine tube and pass between the folds of the broad ligament to be inserted into each labium majus. Round ligaments have little value as a support but they help the broad ligament keep the uterus in place and tend to maintain the anteverted position of the uterus.
- Ovarian Ligaments: arises from the cornua of the uterus but behind the uterine tubes and pass down between the folds of the broad ligament to the ovaries. The round ligament, the ovarian ligament, and the uterine tubes are very similar in appearance and arise from the same area in the uterus.
- Cardinal Ligaments: the chief uterine supports; these ligaments fan out from the sides of the cervix to the side walls of the pelvis, suspending the uterus from the side walls of the true pelvis. They are also called transverse cervical ligaments or Mackenrodt’s ligaments.
- Uterosacral Ligaments: pass backwards from the cervix to the sacrum and support for the uterus and cervix at the level of the ischial spines.
- Pubocervical Ligaments: pass forward from the cervix, under the bladder, to the pubic bones.
The uterus is a primary reproductive organ, functioning for menstruation, pregnancy or gestation, and labor:
- Menstruation: under the influence of the ovarian hormones estrogen and progesterone, the uterine endometrium thickens (proliferative stage), becomes vascular, is ready for implantation (secretory stage), and is then sloughed off if implantation does not take place (menstrual stage).
- Pregnancy/Gestation: housing and nourishment of the baby.
- Labor: contractile tissue for the propulsion of the products of conception into the vaginal canal.
The Oviducts
Also known as the fallopian tubes, these are two muscular canals/tubes 8 to 14 cm (average 10 cm) in length that extends from the uterine cornua to a site near the ovaries; enveloped in the upper fold of the broad ligament. It is the site of normal fertilization (mostly the ampullary portion), and are the ducts through which the ova travel from the ovaries to the uterus.
- They are covered by peritoneum folds that drape down below as broad ligaments and extend at the sides to form the infundibulopelvic ligaments.
- The lumen of the oviducts is lined by a ciliated mucous membrane called the ciliated cubical epithelium. This membrane produces a current of lymph that facilitates the movement of the ovum along the tube.
- The oviducts, as mentioned, are muscular. They rhythmically contract at a rate that varies with hormonal changes in the ovarian cycles.
| Parts | |
|---|---|
| Interstitial Portion | 1.25 cm long and has a lumen that is 1 mm in diameter; embodied within the uterine muscular wall. |
| Isthmus | a narrow portion immediately after the uterus and extends 2.5 cm from it, or about one-third of the length of the tube. |
| Ampulla | the widest portion, 5 cm long and makes up about half of the length of the tube; site of fertilization (conception). |
| Infundibulum | the funnel-shaped passage that has a fringed end that is composed of the fimbriae. One of the fimbriae (the fimbra ovarica/ovarian fimbria) is elongated and connected to the ovary. |
Ovaries
Two almond-shaped organs sized 2.5 to 5.0 cm in length, 1.5 to 3.0 cm in breadth, and 0.6 to 1.5 cm thick. They weigh 6 to 10 grams each, and are situated in the upper part of the pelvic cavity, attached to the posterior surface/back of the broad ligament within the peritoneal cavity.
The ovaries appear smooth with a dull-white surface through which glisten several small follicles; more corrugated in older women and markedly convoluted in elderly women. They consist of three layers:
- Tunica albuginea: dense and dull white; protective layer.
- Cortex: contains the ovarian follicles in different stages of development (ova, Graafian follicles, corpura lutea, degenerated corpora lutea/corpora albicantia, degenerated follicles) held together by the ovarian stroma. There are about 200,000 primordial follicles in the ovarian cortex at birth.
- The inner part of the cortex, the medulla is composed of loose connective tissues, it contains nerves, blood vessels, and lymphatic vessels. The hilum where these vessels enter lies just where the ovary is attached to the broad ligament. This area is called the mesovarium.
- The motor and sensory sympathetic and parasympathetic nerves follow the ovarian artery across the infundibulopelvic ligament to reach the ovary. The ovaries are insensitive unless they are distended and squeezed.
- Mittelschmerz is a mid-cycle pain marked during ovulation when the ovum is released and the Graafian follicle bursts, as the peritoneum becomes irritated by blood or fluid escaping along with the ovum.
The ovaries are the female gonads, and are responsible for both reproductive and endocrine functions:
- Oogenesis: the process of developing a mature ovum in a Graafian follicle. When primordial follicles mature and become cystic, they are termed Graafian follicles.
- Ovulation: the monthly expulsion of a mature ovum from the Graafian follicle into the pelvic cavity.
- Endocrine Function: secretion of female hormones estrogen and progesterone; maturing follicles secrete estrogen, while the corpus luteum secretes estrogen and primarily progesterone.
- Ovaries: primary source of estrogen; adrenal cortex (extraglandular sites) produce a minute amount of estrogen.
- Estrogen: develops female secondary sex characteristics.
- Progesterone: the hormone of pregnancy; its effects on the decidua (thickened and more vascular) allow pregnancy maintenance.
Mammary Glands (Breasts)
Located under the skin, over the pectoralis major muscles. It is made of fibrous, adipose, and glandular tissue. The glandular tissue is arranged in about 15 to 25 lobes. Each lobe is composed of lobules, which in turn are composed of alveoli with secreting cells (acinar cells) that produce milk; and excretory ducts that lead from each lobe to an opening in the nipple composed of erectile tissue and muscle fibers that have a sphincter-like action in controlling the flow of milk. The smooth muscle of the nipple causes the erection of the nipple on contraction.
- The areola is a pigmented area of skin surrounding the nipple.
- Size varies on adipose tissue rather than glandular tissue. Estrogen during puberty develops breast size. Size is not a significant factor in successful breastfeeding.
- Milk secretion (lactation) is used for nourishment and transfer of maternal antibodies. It is also a site of sexual stimulation.
Maternal Reflexes
- Prolactin Reflex: the milk secretion reflex; a high prolactin level stimulates the alveoli, particular the acini cells. Milk is then stored in the breast tubules. High levels of estrogen and progesterone induce alveolar and duct growth as well as stimulate milk secretion. In pregnancy, milk secretion is not stimulated because of low prolactin as a result of high estrogen secretion by the placenta.
- Let-down Reflex: draught reflex; oxytocin-induced flow of milk after stimulation by sucking on a lactating breast. It is also affected by maternal emotions.
- Milk Ejection Reflex: controls the expulsion of milk from the breast tubules, also under the influence of oxytocin secreted by the PPG.
The Menstrual Cycle
Reference
Salustiano, R. (2024). The Menstrual Cycle. In Dr. RPS Maternal & Newborn Care: A Comprehensive Review Guide and Source Book for Teaching and Learning (2nd ed., pp. 50-63). C&E Publishing, Inc.
The menstruation is a series of rhythmic reproductive cycle that begins from the onset of menstrual bleeding to the day before the next bleeding day. It is characterized by changes in the ovaries and the uterus, influenced by normal hormonal variation mediated by the hypothalamus and anterior pituitary gland (APG) via a negative feedback mechanism. This cycle functions to prepare for the release of egg, fertilization, and implantation.
- Begins recurring cyclically at puberty with the first menstruation called menarche and ceasing at menopause.
- The duration of the cycle is highly individualized, but the average/mean cycle length is 28 days; as short as 21 days or as long as 40 days. The regularity of the cycle is also individualized, as some experience irregular (fluctuating length) cycles.
- The only fairly constant interval is the time from ovulation to the beginning of menses, which is almost always 14 to 15 days.
Hormonal Control of the Menstrual Cycle
- Hypothalamic Hormones: the hypothalamus secretes gonadotrophin-releasing (GnRF) or inhibiting factors (GnIF) that stimulate the pituitary gland to secrete or inhibit the secretion of corresponding gonadotrophins (Gn).
- Anterior Pituitary Hormones (APG): the producer of gonadotrophins (Gn), follicle-stimulating hormones (FSH), and luteinizing hormone (LH).
- FSH is secreted in response to the hypothalamic follicle-stimulating hormone releasing factor (FSHRF) triggered by low blood levels of estrogen during the first half of the menstrual cycle. Estrogen, by the fourth to fifth day, is at its lowest in a regular 28-day cycle.
- LH, also called interstitial-cell stimulating hormone, is secreted in response to the hypothalamic luteinizing hormone releasing factor (LHRF) triggered by low blood levels of progesterone. Progesterone, by the thirteenth day, is at its lowest. Progesterone is responsible for the rise in basal body temperature found on the fourteenth day, and the drop on the thirteenth day in a regular 28-day cycle.
- Ovarian Hormones: Estrogen and Progesterone
- Estrogen is secreted by the ovaries, adrenal cortex, and placenta (during pregnancy).
- It is responsible for the development of secondary sexual characteristics
- Assists in the maturation of ovarian follicles
- Inhibits secretion of FSH (negative feedback)
- Stimulates secretion of LH (positive feedback)
- It is responsible for the proliferative phase of the menstrual cycle.
- It is responsible for the fertile cervical mucus that is conducive to fertilization; the change of cervical mucus to thin, clear, colorless, stringy, stretchable, slippery, and lubricative, returning a positive ferning test.
- In pregnancy, it increases vascularization, maintains the highly-specialized endometrium (decidua), stimulates uterine muscle contraction, causes fatigue, and antagonizes insulin.
- Progesterone is secreted by the corpus luteum (non-pregnant/early pregnancy) and placenta (as early as the sixth week of pregnancy until parturition)
- Inhibits secretion of LH (negative feedback)
- Helps maintain the endometrium by facilitating the secretory phase of the menstrual cycle in preparation for nidation (implantation)
- Relaxes smooth muscles, including the myometrial muscle of the uterus:
- Maintains pregnancy by maintaining decidua. If progesterone levels drops in pregnancy, abortion (early pregnancy) or premature labor (late pregnancy) may occur.
- One of the main theories of labor onset is when progesterone levels drop at term, giving way for the myometrium to contract easily from stimulation by rising stimulants such as oxytocin and prostaglandin.
- Increases body temperature (Thermogenic)
- Water-retaining, anti-diuretic action; decreases hemoglobin and hematocrit levels
- Increases fibrinogen level, increasing coagulability
- Responsible for infertile cervical mucus: thick, opaque, sticky, non-stretchable
- Antagonizes insulin along with estrogen, human placental lactogen (HPL), and cortisol.
- Estrogen is secreted by the ovaries, adrenal cortex, and placenta (during pregnancy).
- Prostaglandin: fatty acids recognized as a hormone secreted by a lot of body organs, including the endometrium of the uterus. This affects the menstrual cycle and contributes to stimulating uterine muscles for contraction
Stages/Phases of the Menstrual Cycle
- Menstrual Phase or the Bleeding Phase, also known as menstruation. Day 1 to 4, lasting for 3 to 5 or 4 to 6 days. It is the terminal phase of the cycle.
- Characterized by vaginal bleeding as the uterine endometrium is shed down to the basal layer along with blood from the capillaries and with the unfertilized ovum.
- Periodic discharge of blood, mucus, and cellular debris from the uterine mucosa and occurs at regular, cyclic, and predictable intervals from menarche to menopause.
- The period of absolute infertility
- Menarche is the first onset of menstruation, occurring between 12 to 13 years of age; usually anovulatory, infertile, and irregular.
- 25 to 60 mL of blood, with about 0.4 to 1.0 mg of iron is lost every day.
- Menstrual blood is incoagulable due to fibrinolytic activity.
- Follicular/Proliferative Phase: Day 5 to 14, ending in ovulation; lasts about 9 days.
- This phase is controlled by estrogen, where the endometrium thickens by 8 to 10 times during the first few days, known as the regenerative phase.
- After changes level off at ovulation, the endometrium consists of three layers:
- Basal Layer: 1 mm, thick, never alters
- Functional Layer: 2.5 mm, contains tubular glands, consistently changes according to hormonal influences of the ovary
- Cuboidal Ciliated Epithelium Layer: uppermost layer, covers the functional layer, and dips down to line the tubular glands
- Ovulation is present in the middle of the cycle; monthly growth and release of a mature, non-fertilized ovum from the ovary. It is the period of absolute fertility. This usually occurs 13 to 15 (average of 14) days prior to the next cycle. At this point, estrogen is high while progesterone is low.
- Signs of ovulation include breast tenderness, slight rise in BBT (0.3°C to 0.5°C; 0.4°F to 0.8°F) preceded by a slight drop (0.2°F) 24 to 36 hours before, related to changes in progesterone levels.
- The most fertile time is 3 to 4 days before and 1 to 2 days after ovulation.
- Positive Spinnbarkeit/Creighton/Billings/Cervical Mucus Test
- Mittelschmerz, left or right lower quadrant pain corresponding to the rupturing of the Graafian follicle.
- Positive Ferning Test
- Estimating ovulation time: subtract 14 days from the menstrual cycle length e.g. it occurs on the 14th day in a 28-day cycle, and on the 16th day in a 30-day cycle.
- The period of fertility is calculated as five days before and two days after the day of ovulation. In a 28-day cycle, the period of fertility is from 9 to 17th day counting from the first day of bleeding.
- Luteal/Secretory Phase: Day 15 to 28; lasts about 12 days.
- This phase is initiated by ovulation in response to a surge in LH that promotes the development of corpus luteum from the ruptured follicle, the yellow body that secretes high levels of progesterone and estrogen.
- Progesterone stimulates the already-proliferated endometrium, causing the functional layer to become thicker (2.5 mm → 3.5 mm), more spongy, and softer with glands becoming more tortuous as the endometrial capillaries get distended with blood in preparation for reception/implantation and nourishment of the fertilized ovum.
- If fertilization occurs, implantation follows 6 to 9 or 7 to 10 days (average 7 days) after. The corpus luteum lives longer and secretes progesterone and estrogen in early pregnancy, which is later replaced by the placenta. The normal lifespan for the corpus luteum is 10 to 14 days.
- If fertilization does not occur, the corpus luteum involutes after 7 to 8 days after ovulation, becoming white (corpus albicans) which persists up to 10 to 12 days after ovulation. This causes a drop in estrogen and progesterone, leading to the endometrial ischemic/premenstrual phase.
Fertilization and Fetal Development
Reference
Salustiano, R. (2024). Fertilization and Fetal Development. In Dr. RPS Maternal & Newborn Care: A Comprehensive Review Guide and Source Book for Teaching and Learning (2nd ed., pp. 64-79). C&E Publishing, Inc.
Fertilization (conception, fecundation, impregnation) is the union of a mature egg cell (ovum) and sperm cell in the ampulla (outer third) of the fallopian tube. The resulting fertilized egg is called the zygote.
Sperm move within the female reproductive system through flagellar action. Each sperm often reach the ampulla within 5 minutes, up to 4 to 6 hours after ejaculation. From 400 million or more sperm, only ~200 actually reach the ampulla. Sperm often remain for 4 to 6 hours before being able to fertilize an egg, as this period is when sperm capacitation and acrosomal reaction occurs:
- Sperm Capacitation: the sperm becomes hypermobile, and the acrosomal membrane/covering of the sperm head becomes exposed, allowing it to bind with the zona pellucida of the ovum.
- Acrosomal Reaction: the deposition of minute amounts of hyaluronidase in the corona radiata, allowing the sperm to penetrate the ovum.
As soon as the sperm penetrates the zona pellucida and makes contact with the vitelline membrane of the ovum, a cellular change occurs in the ovum that inhibits other sperm cells from entering. This process is mediated by the release of materials from cortical granules (organelles) just under the egg surface.
Fertilization occurs when the male pronucleus units with the female pronucleus; thus, the chromosome diploid number (46) is restored and a new cell, the zygote, is created with a new combination of genetic material, which creates a unique individual different from the parents and anyone else.
The zygote undergoes cleavage/mitosis, in sequential order:
- Zygote: the cell that results from fertilization of the ovum by a spermatozoa. This cell undergoes mitosis, which is the process of cell replication where each chromosome splits longitudinally to form a double-stranded structure.
- Cleavage: a series of mitotic cell divisions by the zygote
- Blastomere: daughter cells arising from the mitotic cell division of the zygote (2-cell, 4-cell, and 8-cell blastomeres).
- Morula: a solid ball of cells produced by 16 or so blastomeres; called the “traveling” form because it is in this form when it migrates through the fallopian tube (oviduct) and reaches the uterine cavity about 3 to 4 days after fertilization.
- Blastocyst: a fluid-filled cavity that reaches the uterine cavity.
Morula Reformation
The morula reforms to become the blastocyst; the cavity within the morula is the blastocoele. This cavity expands, and the outer cells of the morula become the trophoblast. It is after this reformation that energy becomes necessary, and the blastocyst implants into the uterine wall for further development.
Implantation, also known as nidation, occurs within 6 to 9 days (average 7 days) after fertilization. In a normal implantation, the site is in the upper fundal portion or upper one-third of the uterus, either anteriorly or posteriorly. Abnormal implantation sites are the fallopian tubes (ectopic pregnancy) and the lower uterine segment (placenta previa).
Blastocyst
While the blastocyst is in the stage of implantation, its outer layer, the trophoblast, is responsible for actual implantation (nidation). The trophoblast gives rise to the placenta.
The Placenta
The placenta is a discoid (15 to 20 cm in diameter by 2 to 3 cm thick) product of conception in the uterus, positioned anteriorly or posteriorly near the fundus. Its base is always where the site of implantation occurs. It consists of two sides, the fetal side and the maternal side:
- Fetal Side: covered with amnion; under which fetal vessels course with the arteries passing over the veins. An amnion is 0.02 to 0.5 mm in thickness, a sac that engulfs the growing fetus. The clear fluid that accumulates within the amniotic cavity is the amniotic fluid.
- Maternal Side: irregular lobes consisting of fibrous tissue with sparse vessels confined mainly to the base.
By the time the pregnancy reaches term, the placenta is, on average, 500 grams in weight. The weight-ratio at term in an average fetus and placenta (feto-placental weight ratio) is 6:1 (3,000 grams to 500 grams).
The placenta forms with the union of the chorionic villi and the desidua basalis. The Decidua is the endometrium during pregnancy; thickening to 5 to 10 mm. It consists of multiple layers and sublayers:
- Decidua Basalis: the base layer, under the embedded ovum, directly under the site of implantation.
- Decidua Capsularis: the portion overlying the developing ovum; separates the ovum from the rest of the uterine cavity; most prominent by the second month.
- Decidua Vera/Desidua Perietalis: lines the remainder of the uterus.
Placental Maturity
The placenta begins developing within the second month of pregnancy, and becomes completely functional on the third month of gestation. It functions most effectively through 40 to 41 weeks, and may be dysfunctional beyond 42 weeks.
Placental functions vary, and play vital roles in nutritive, respiratory, excretory, protective, and endocrine systems:
- Nutritive: transports nutrients and water-soluble vitamins to the fetus via fluid/gas transport.
- Respiratory: serves as the fetal organ of respiration.
- Excretory: the amniotic fluid is the medium of excretion.
- Protective: the placental barrier defends against organisms and substances like heparin and bacteria. It is ineffective against viruses, alcohol, nicotine, antibiotics, depressants, and stimulants.
- Endocrine: production of estrogen, progesterone, human chorionic gonadotropins (hCG), and human placental lactogen (hPL), also called chorionic somatomammotropin (hCS).
- The major source of estrogen and progesterone after the first two months.
- hCG: secreted as early as 8 to 10 days after fertilization, detected in serum as early as the time of implantation by the most sensitive pregnancy test, radioimmunoassay (RIA). Detected in urine by 10 days (2 weeks) after the first amenorrheic period. It prolongs the lifespan of the corpus luteum, and serves as the basis of pregnancy tests. It is found to be elevated in cases of excessive vomiting. Normally, its value is 50,000 to 400,000 IU/24 hours.
- hCS/hPL: secreted by the third week after ovulation, influencing somatic cellular growth (resembling growth hormone). It is the principal diabetogenic factor, being a major insulin antagonist/glucose sparing hormone. It prepares the breasts of the mother for lactation.
Placental/Cord Abnormalities
- Placenta succenturiata: the presence of accessory lobes of the placenta.
- Placental infarcts: the death of a portion of the placenta, often due to ischemia.
- Placenta bipartita: a bilobed placenta, a placenta that develops into two roughly equal-sized lobes separated by a membrane.
- Placenta tripartita: a trilobed placenta, a placenta that develops into three roughly equal-sized lobes separated by membranes.
- Placenta circumvallata: the membranes of the placenta fold back around its edges.
- Battledore placenta: marginal cord insertion, where the umbilical cord is inserted at or near the placental edge/margin rather than in the center.
- Velamentous insertion of the cord: an abnormality of the cord where the umbilical vessels diverge as they traverse between the amnion and chorion before reaching the placenta.
- Cord loops: twisting of the umbilical cord around the fetus, especially the neck.
- Cord torsion: excessive twisting can result in torsion, which can lead to fetal demise. Most cases of cord torsion is only found upon pathological examination.
- Cord knots: the knotting of the cord, which compromise blood flow.
The Umbilical Cord
Also known as the funis, it is a 30 to 100 cm (average 55 cm) cord with a diameter of 0.8 to 2.0 cm at term. It extends from the fetal surface to the placenta to the fetal umbilicus, serving to transport oxygen and nutrients, and returning metabolic wastes from the fetus to the placenta. It contains three umbilical vessels (mn. AVA): one vein and two arteries.
- Umbilical Vein: carries oxygenated blood to the fetus.
- Umbilical arteries: carries deoxygenated blood from the fetus to the placenta.
Protective Covering of the Funis
The cord is covered by Wharton’s Jelly, a specialized gelatinous connective tissue, an extension of the amnion that prevents cord compression.
The Amniotic Fluid
A clear, straw-colored fluid in which the fetus floats. It appears from both the fetal and maternal placenta, amniotic epithelium, maternal serum, and in the latter part (10th week), fetal urine. It is continuously replaced to prevent “dry labor” in a premature rupture of the bag of water. It reaches 500 to 1,000 mL. More than this results in polyhydramnios (1,000 to 1,500 mL), and less results in oligohydramnios (300 to 500 mL). Its pH is normally neutral to alkaline (pH 7.00 to 7.25).
It functions as a protective cushion/shock absorber. It separates the fetus from membranes, allowing symmetrical growth and free movement. As previously mentioned, it is the medium by which wastes are excreted from the fetus. It also serves as a fetal drink.
- The amniotic fluid can be used as a specimen for periodic diagnostic exams (amniocentesis) to determine fetal well-being or its absence.
- Fetal temperature is also maintained by amniotic fluid.
- The liquid prevents marked interference with placental circulation during labor.
Abnormalities
- Polyhydramnios: an elevation in amniotic fluid volume, over 1,000 mL.
- One of the causes of polyhydramnios is when the fetus is unable to drink; if an abnormality in the deglutition center of the brain or if there is esophageal atresia that the fetus cannot swallow.
- Oligohydramnios: a decrease in amniotic fluid volume, under 500 mL.
- Meconium-stained amniotic fluid, especially if the fetus is non-breech, is a sign of fetal distress.
- Golden-colored amniotic fluid may be found in hemolytic disease.
Intrauterine Growth and Development
| Age | Development (RPS) | Short Ver. (Sir V.) |
|---|---|---|
| 4 weeks | All systems in rudimentary form: beginning formation of eyes, nose, and GIT Partitioning of the primitive heart begins; heart chambers are formed; the heart beats (14 days); the heart is completely formed by the end of 6 weeks With arm and leg buds By the end of the 4th week after ovulation, the chorionic sac is 2 to 3 cm in diameters, and the embryo is about 4 to 5 mm in length | - Dizziness due to nervous system development of the fetus. For this, glucose is the foremost requirement. This results in the slight hypoglycemia of the mother that results in dizziness. - Fetal Heart Beat begins 16 days after conception. |
| 8 weeks | Head size is large in proportion to the body, neuromuscular development, and some movements. Rapid brain development External genitalia appear | - Sex Differentiation (6th week) - Fetal Heart Tone auscultation with a doppler, unheard with a stethoscope. - Placental development (not fully functional) |
| 12 weeks | Placenta fully formed Functioning kidneys develop, secrete urine Centers of ossification in most bones With sucking and swallowing Gender distinguishable FHT detected by ultrasound (10 to 12 weeks) Crown-rump fetal length is 6 to 7 cm. Uterus is palpable just above the symphysis pubis | - Placenta is fully functional - Renal system becomes functional. This is when the fetus begins to urinate in-utero. |
| 16 weeks | More human appearance Quickening felt by the multigravida Meconium in the bowels External genitalia are obvious; gender correctly determined by experienced observers by inspection of the external genitalia at 14 weeks (Cunningham et al., 2022) Scalp hair develops Formed eyes, nose, and ears FHT detected by fetoscope By the end of 16 weeks, crown-rump length is 12 cm, and fetal weight is 110 g | - Sex Differentiation is complete, but the external genitals remain small, which may lead to false determination. - Fetal Heart Tone auscultation with a fetoscope. - Lanugo: fine downy hair on the shoulder, nape, arms, etc. - Quickening: first fetal movement felt by multiparous women. - IgG transfer from mother to fetus |
| 20 weeks | Skin is less transparent With vernix caseosa and downy lanugo covering the entire body Quickening is stronger, felt by the primigravida FHT is audible using a stethoscope Bones are hardening Weight is more than 300 g | - The best period for sex determination through ultrasound. - Vernix caseosa appears: the cheese-like substance for lubrication during delivery. - Fetal Heart Tone auscultation with a stethoscope. - Quickening: first fetal movement felt by primiparous women. |
| 24 weeks | Weight is about 630 g Body is well-proportioned Skin is red and wrinkled; fat deposition begins Hearing established Eyebrows and eyelashes are recognizable Canalicular period of lung development. When born, some may breathe, but most will die because the terminal sacs required for gas exchange have not yet formed | - Surfactant Production for alveolar lubrication. - Hearing ability develops: the best time to start singing or talking to the fetus. |
| 28 weeks | Weight is 1,100 g. The crown-rump length is about 25 cm Viable; immature if born at this time; surfactant production begins Thin skin, red, covered with vernix caseosa Body less wrinkled With iron storage Nails appear The pupillary membrane has just disappeared from the eyes | - Bone Ossification: fetal bone development. Calcium demand increases. This results in leg cramps for the mother. Premature occurrence of leg cramps indicate inadequate calcium intake. (Vitamin D increases Calcium absorption; Vitamin C increases Iron absorption). |
| 32 weeks | Weight is 1,800 g. The crown-rump length is about 28 cm Subcutaneous fats begin to deposit; the skin is smooth and pink More reflexes (moro) are present With iron and calcium storage Good chance of survival if delivered at this stage | - Iron is transferred to the fetus. - Ultrasound at this period shows high presence of calcium in the base of the placenta. Calcium may be visualized (placental grading) due to the clumping of calcium with each other. - Lanugo disappears. |
| 36 weeks | Weight is 2,500 g. The crown-rump length is about 32 cm Lecithin/sphingomyelin (L/S) ratio is 2:1. Nails firm With a definite sleep/wake pattern More rotund body because of subcutaneous fat deposition Lanugo disappearing Excellence chance of survival with proper care; survival is the same as term | - Vernix caseosa disappears. |
| 40 weeks | Weight: approximately 3,400 g. Crown-rump length is 36 cm Full-term, fully developed, with good muscle tone and reflexes Little lanugo If male, testes in the scrotum The age at the time of EDC counts from first day of LMP With other characteristic features of the newborn |
Family Planning
Planning the number of family members in terms of timing, number, and interval between children, mainly achieved through contraception. There are natural forms and artificial methods.
Natural Methods
- Abstinence: primarily countered by self-control.
- Strict: absolute abstinence from any form of intercourse.
- Regular: no vaginal intercourse, permitting other forms of intercourse.
- Lactational Amenorrhea Method (LAM): provides protection for 6 months after delivery when observing exclusive breastfeeding via maintenance of high estrogen levels, which inhibits the release of FSHRF, therefore inhibiting FSH, the hormone responsible for maturation of egg cells. (Breastfeeding → High Estrogen → Low FSHRH → Low FSH → Non-maturity of Egg Cells)
- Breastfeeding may be combined with pills when the 6 month period runs out.
- Fertility Awareness Method (FAM): the Father and Mother should both receive counselling for education about family planning.
- Calendar Method:
- Ask the patient if they are regular or irregular.
- If regular, ask the patient about the duration of their cycle. To get their window of fertility, deduct 14 from the length, then extend three days back and five days forward.
- 30 day duration → → 11th to 19th day after the onset of menstruation.
- If irregular, find the longest cycle and shortest cycle:
- The fertile window of the patient is bordered by these values; ex. a patient with 21 to 36 day cycles would have a fertile window of 3rd to 25th day after onset of menstruation.
- Cervical Mucus Test/Billing’s Test/Spinnbarkeit/Creighton’s Method:
- The cervical mucus is dry during periods of infertility, and wet during periods of fertility.
- ex. in a 28 day cycle, the mucus is dry on days 6 to 8, and 18 to 28.
- The characteristics of a fertile cervical mucus are: watery, abundant, thin, clear, elastic, and slippery.
- Cervical mucus is collected in the morning, observed after arising from the bed.
- Rub the mucus between the thumb and index, then attempt to stretch it. If it stretches 5 to 10 cm without breaking (and is therefore thin), the woman is likely fertile.
- Basal Body Temperature (BBT) Test: a woman’s BBT increases with high levels of progesterone. Temperature is taken before getting out of bed to avoid increasing BBT from activity and eating. Contraindicated in febrile women and those who are unable to obtain a thermometer. In a 28-day cycle with ovulation on the 14th day:
- 3rd: low estrogen; 13th: high estrogen
- 13th: low progesterone; a sudden decrease in temperature
- 14th: high progesterone; a sudden increase in temperature. Temperature shifts by 0.2C to 0.5C.
- ex. d11: 36.7 → d12: 36.7 → d13: 36.5 → d14: 37.0 → d15: 37.0 → d16: 37.0 → d17: decr.
- Symptothermal Method: a combination of CMT and BBT.
- 2-day Method: a replacement of the CMT for patients who are against collecting their cervical mucus. For the 2-day method, compare the cervical mucus for the past two days; if two consecutive days are dry (D), the woman is infertile. When a wet (W) period exists within a two day period, the woman may be fertile i.e. DD is okay, DW, and WD, and WW are not.
- Calendar Method:
Artificial Methods
- Hormonal: prevention of pregnancy through ovulation suppressants which act to prevent hypothalamic activity for FSHRF and LHRF by elevating hormone levels.
- Pills: hormone-containing oral supplements for synthetic hormones.
- Progestine Only Pills (POP): progesterone only pill, containing 21 tablets. The patients take the pills daily, then wait for seven days. After, on the 29th day, start a new pack.
- Allowed in breastfeeding.
- Combined Oral Contraceptive Pills (COC; COCP): a combination of progesterone and estrogen, given in 28 tablet parts. 21 are white (containing hormones), and 7 are brown (placebos). The best time to start taking the pills is during menstruation; first pill on the first day of menstruation.
- When taking the brown tablets, menstruation ensues, often on the second or third pill. The woman may also reject the brown pills. Instead, mark or dispose of them to not lose track.
- Not used in breastfeeding, as estrogen decreases milk production.
- Estrogen is a vasoconstrictor, and is therefore not used in hypertension, smokers, >35 years old, diabetics, heart disease, thrombolytic, and liver problems.
- Not used when pregnant.
- Danger Signs: (mn. JACHES)
- Jaundice, Abdominal Pain: from liver problems
- Chest Pain: heart disease
- Headache and Eye Problems: HTN
- Severe Leg Pain: Thromboembolytic Disease
- Forgetting/Skipping Doses:
- Forgot in the set time for the day: take the pill on the same day
- Forgot one day: take two pills the next day.
- Forgot two days: take two pills the next day, then two the day after that.
- Forgot three days: discard the pack.
- Progestine Only Pills (POP): progesterone only pill, containing 21 tablets. The patients take the pills daily, then wait for seven days. After, on the 29th day, start a new pack.
- Injectable: Defoprovera, a progesterone-based injectable received during menstruation. It provides protection for three months.
- Do not massage the injection site as this hastens its absorption rate, shortening the duration of protection. Only press on the injection site.
- There will be no menstruation during this period.
- Implant: Implanon, a 99.98% effective method; the most protection. It is progesterone-based, and provides protection for three years.
- A large number of women remove their implant due to associated weight gain.
- There will be no menstruation during this period.
- Patch: Orthoevra; three patches that last 7 days (21 days total) then cessation for 7
- Patches are applied on the arm or thigh; highly muscular areas.
- Pills: hormone-containing oral supplements for synthetic hormones.
- Barrier: prevents the sperm from entering into different parts of the reproductive system. The condoms and CC/D are latex.
- Condom: prevents entrance into the vaginal canal.
- Protects against HIV/AIDS, Gonorrhea, but NOT genital warts, herpes, and pediculosis.
- Cervical Cap/Diaphragm: prevents entrance into the cervical canal. These are combined with spermicide to have improved effectivity.
- The use of a condom is contraindicated, as friction may damage both contraceptives. The woman is no longer protected from STDs.
- After ejaculation, the cervical cap is not to be manipulated or removed 6 to 8 hours after ejaculation, but not to be retained for more than 24 hours. If maintained for longer, Toxic Shock Syndrome results, often caused by E. coli and Staphylococcus aureus resulting in diarrhea and respiratory infection respectively.
- IUD: prevents entrance into the fallopian tubes. The most common form is the Copper T IUD, inserted during menstruation to ensure the woman is not pregnant. This IUD may stay within the uterus for 10 years.
- The most common problem with IUDs is the displacement or expulsion of the IUD, often presenting as pain.
- An IUD, if placed before pregnancy, may coexist with a pregnancy.
- Condom: prevents entrance into the vaginal canal.
- Chemical; Spermicides: only 80% effective; the least effective.
- Tablet
- Foam
- Gel
- Spray
- Sponge, a combination of barrier and chemical
- Surgical
- Vasectomy:
- Protection against STDs is present, but not all forms e.g. warts and genital herpes.
- Bilateral Tubal Ligation (BTL):
- Vs. IUD:
- Menstruation is maintained in both.
- Ovulation is maintained in both.
- Protection against pregnancy is present in both, and both also fail to protect against STDs.
- BTLs are permanent. IUDs are temporary.
- Both are done during menstruation.
- Vs. IUD:
- BRAIDED Counselling:
- Benefits: e.g. BTL is hassle-free.
- Risks: minor surgeries introduce risk for bleeding and infection, both manageable.
- Alternative methods
- Inquiries/concerns
- Declining is respected
- Explanation of procedure, ideally from the physician
- Documentation: informed consent forms for the surgery and sterilization
- Vasectomy:
The Antepartal Period
Reference
Salustiano, R. (2024). The Normal Antepartal Period. In Dr. RPS Maternal & Newborn Care: A Comprehensive Review Guide and Source Book for Teaching and Learning (2nd ed., pp. 80-116). C&E Publishing, Inc.
The antepartal period is the period of pregnancy or the period before labor, also called the prenatal or the antenatal period. The woman in this period is called the gravida. It is part of the perinatal period, extending from one year before to two years after (18-24 months) giving birth.
Duration of Pregnancy
A normal pregnancy lasts for 267 to 280 days; 9 calendar months; 10 lunar months; 40 weeks; or 3 trimesters. The best measurement for gestational age (AOG) and length of pregnancy is weeks. The expected date of confinement (EDC) is at 40 weeks AOG.
- First Trimester: the period of rapid organogenesis, where teratogens (alcohol, drugs, viruses, and radiation) cause the most damage.
- Second Trimester: the most comfortable period, with continued growth of the fetus.
- Third Trimester: rapid deposition of fats, iron (8th month), and calcium (7th month), as the period with the most rapid fetal growth.
Physiological Adaptations in Pregnancy
Reproductive System
The Uterus grows from 7.5 × 4 × 2.5 cm, pyriform/pear-shaped to 32 × 24 × 22 cm, globular/oval. Its weight increases from 60 ~ 70 grams to 1,000 grams. Despite this, no new uterine muscle is formed. The existing muscle fibers become hypertrophic, and new fibroelastic tissues form to make stronger uterine walls. Changes are progressive.
- 12 weeks: the corpus and fundus become globular; almost spherical.
- Fundal Height is at the level of the symphysis pubis until the 12th week, and is generally only palpable by the 13th week just above the symphysis pubis. It reaches the umbilicus by the 20th to 22nd week, and the xiphoid process by the early 36th week. This is also expressed in Bartholomew’s Rule.
- Increased vascularity (because of Estrogen) results in three probable signs of pregnancy:
- Hegar’s Sign: softening of the isthmus.
- Goodell’s Sign: softening of the cervix
- Chadwick’s Sign: blue/purple discoloration of the cervix and vaginal mucosa. This may also be seen as a presumptive sign of labor as observed by the pregnant woman.
- Braxton Hicks Contractions: intermittent, irregular, painless, abdominal, and false labor contractions felt by 4 months, and is more pronounced on the 8th month.
- Ballottement: rebounding of the fetal head against examining fingers by 4 to 5 months (16th to 18th week of gestation). This is felt by healthcare examiners on the third Leopold’s Maneuver (Pawlick’s Maneuver).
- Secondary Amenorrhea: often the first sign that alerts a woman to pregnancy; the lengthened lifespan of the corpus luteum (from two weeks to two months) prevents another menstrual period to initiate.
- Uterine Electrical Activity: low and uncoordinated in early gestation, progressively intensifying and synchronizing at term. This synchronization occurs twice as fast in multiparas.
The cervix becomes shorter, thicker, and more elastic. Its mucosal lining increases mucus production (from edema and thickening), which creates the mucus plug by week 7 that protects the uterus from bacterial contamination. As previously mentioned, this is also subject to Chadwick’s Sign, becoming discolored to blue/purple from increased vascularity. The vagina also becomes thicker and hypertrophic, thickening the vaginal mucosa. Leukorrhea occurs as whitish, mucoid, non-foul, non-pruritic vaginal secretions increase along with estrogen. Vaginal acidity increases, adding protection against bacterial invasion.
Ovulation and maturation cease as the ovaries’ function is overtaken by the corpus luteum in early pregnancy; it functions maximally during the first 6 to 7 months of pregnancy.
The breasts increase in size and firmness. The areola and surrounding skin darkens and enlarges, along with the alveoli system, alveoli duct, and Montgomery’s glands. Superficial veins enlarge and become prominent. Breastfeeding can be done as early as 4 to 5 months (for other infants, if needed), as colostrum begins to be produced.
Endocrine System
The major endocrine organ during pregnancy is the placenta. Its chorion (15 to 20) secrete Human Chorionic Gonadotropins (hCG) which (a) maintain the corpus luteum by secreting progesterone in early pregnancy, its most important function, and (b) aids in diagnosing pregnancy, as it is detectable in serum (by 8 to 10 days after implantation) and urine (by 10 to 14 days after first missed menstruation). hCG is found to be elevated in pregnant women experiencing vomiting.
- The placenta matures by 10 to 12 weeks (3 months), increasing placental hormones estrogen, progesterone, hCG, and hPL/hCS (Human Placental Lactogen/Human Chorionic Somatomammotropin).
hPL is the major diabetogenic hormone in pregnancy, contributing to gestational DM.
The anterior pituitary gland becomes ready for breastfeeding through increased prolactin. FSH production from the APG does not result in ovulation. The posterior pituitary gland (PPG) secretes oxytocin from the hypothalamus when fetal head pressure on the cervix increases. Oxytocin acts to stimulate the uterine myometrium, causing uterine contractions and labor onset, especially with the decrease in progesterone, which inhibit contractions, in late pregnancy.
Signs of Pregnancy
The signs of pregnancy are divided into three categories. Presumptive signs are those felt by the mother herself, probable signs are those observed by a healthcare provider, and positive signs are those emanating from the fetus itself.
Presumptive Signs
Presumptive signs are subjective; may be noticed by the women but are not conclusive proof of pregnancy, which are:
- Amenorrhea: first sign at two weeks from fertilization because of persistence of corpus luteum.
- Urinary Frequency: most disturbing sign, especially in the third trimester.
- Breast Changes: tingling of the nipples (4 weeks), darkening and enlargement of areola, enlargement of the breasts, and increased number of milk-secreting cells.
- Quickening, often felt stronger at 10 weeks.
- Chadwick’s sign: blue/purple discoloration of the vaginal mucosa/perineum as observed by the woman.
Probable Signs
Probable signs are objective as noticed or observed by the healthcare provider but still not conclusive of pregnancy, which are:
- Abdominal enlargement from uterine growth.
- Goodell’s sign: softening of the cervix.
- Hegar’s sign: softening of the isthmus (lower uterine segment) and compressibility of the uterus.
- Chadwick’s sign: blue/purple discoloration of the cervix, vaginal mucosa, and perineum.
- Ballottement: rebound of the fetus against examining fingers.
- Positive pregnancy test: due to the presence and rising levels of hCG in maternal blood and urine. This may still be a false positive, e.g. in a hydatidiform mole that produces hCG.
Positive Signs
Positive signs are objective; emanate from the fetus; conclusive for pregnancy, which are:
- Fetal Heart Tones (FHT)
- Fetal Outline (upon UTZ)
- Fetal Parts (examiner palpation)
- Fetal Skeleton, as seen via x-ray imaging (not to be done before 16 weeks due to unsafe exposure to radiation).
- Quickening felt by the examiner.
Common Discomforts of Pregnancy
| Discomfort | Cause | Relief Measures |
|---|---|---|
| Morning Sickness | Progesterone effect | - Eat dry crackers (or toast) 30 minutes before arising in the morning. - Eat small, frequent meals and avoid fatty, acidic, and highly seasoned foods. - Drink adequate fluids between meals. |
| Pyrosis | Progesterone effect, gastric compression by the gravid uterus | - Bend at the knees when picking things up off the floor. - Remain upright for 3 to 4 hours after eating. - Avoid taking sodium bicarbonate. Take aluminum-bearing antacids as ordered. |
| Constipation | Progesterone effect, particularly of GI relaxation and decreased motility. | - Increase fluids and fiber. - Increase activity/exercise. - Establish a bowel movement routine/schedule. - Drink warm water in the morning. |
| Urinary Frequency | Pressure on the bladder by the gravid uterus, relieved during the second trimester. | - Increase fluids to replace losses, except for bed time to prevent nocturia. |
| Leg Cramps | Calcium-phosphorus imbalance from fetal bone ossification (7th month). | - Increase dietary calcium, with Vitamin D. - Avoid prolonged standing and sitting. - Dorsiflex the foot, extend the knee to hyperextend the involved muscle. |
| Varicosities | Pressure on the femoral vein and inferior vena cava by the gravid uterus. | - Avoid round garters around the abdomen and legs (knee-high stockings). - Wear a supportive (hip-high) panty hose. - Frequent elevation of the legs and hips is advised. |
| Edema | Increased aldosterone (salt-saving, water-retention) and pressure on the inferior vena cava. | - Assume a left-lateral position or elevate the legs frequently to promote venous return. Avoid prolonged standing. - No round/constricting garters. -Report swelling of the hands and face. Edema should predominantly be pedal. |
| Vena Caval Syndrome | A.K.A. Supine Hypotension Syndrome. Caused by vena caval pressure from the gravid uterus, decreasing cardiac output | - Avoid sudden changes in position. - Avoid staying supine. - Arise from the bed gradually, with a lateral position. - Avoid staying in one position for long periods. - Assume frequent left-lateral positions in bed. |
| Backache | Forward-shifting of the center of mass results in lordosis, and pressure on the bones and ligaments. | - Maintain good posture. Avoid prolonged standing. -Wear flat shoes. -Engage in regular, gently physical activity. - Use a supportive mattress. - Wear a maternity girdle in selected situations as recommended. |
| Shortness of Breath | Pressure on the diaphragm by the gravid uterus. | - Maintain good posture. - Avoid fatigue. - Elevate the head with several pillows; avoid supine position. - Avoid constricting clothing and brassieres. - Report increasing dyspnea at rest prior to 36 weeks. |
Prenatal Management
Prenatal checkups are done to improve maternal and neonatal outcomes. It aims to define the health status of the mother and fetus, the gestational age of the fetus and the estimated date of confinement (EDC), initiate a nursing care plan for continuing maternity care for both the mother and the fetus, and detect any high-risk conditions early. The first visit should be held as soon as the mother misses a menstrual period when pregnancy is suspected. Following this, the schedule of visits are:
| Trimester | DOH (4 total visits) | WHO (14 total visits) | RPS (14 total visits) |
|---|---|---|---|
| 1st Trimester | Once before the fourth month | Once a month | Once a month |
| 2nd Trimester | Once before the sixth month | Once every two weeks | Once a month |
| 3rd Trimester | Once before the eighth month | Once a week | Once a month (to 8th month), then twice a month for the third month |
| Final Month | Once on the final month | Once | Once a week on the final month (36th to 40th week) |
| Frequency increases if danger signals are present, or if known risk factors are established. |
Conducting Visits
Prenatal visits are done to serve as a basis for comparison (baseline data collection) with information gathered on subsequent visits. These function to screen for risk factors during pregnancy. For the initial visit, obtain the woman’s:
- Obstetrical History:
- Menstrual History: menarche, regularity, duration, frequency, character
- Last Menstrual Period, Sexual History, and Methods of Contraception
- Past Menstrual Period
- Medical and Surgical History: past illnesses, surgical procedures, and drugs currently being used.
- Family History: to detect illnesses or conditions that are transmissible or hereditary.
- Current Problems: activities of daily living, discomforts, danger signs.
- Vital Signs: temperature, cardiac rate, respiratory rate, blood pressure
- Temperature becomes elevated by progesterone and basal metabolic rate, not to reach 38°C.
- Cardiac rate increases by 10 to 15 BPM during pregnancy.
- Respiratory rate at rest can increase to 24 respirations/min.
- Blood pressure is rarely affected, but hypotension can occur due to supine hypotension syndrome/vena caval syndrome. Prevention of this syndrome is through the use of a left-lateral recumbent position. Pregnancy-Induced Hypertension (PIH) is an important problem of pregnancy.
- The roll-over test can be done in the first trimester for early detection of developing PIH by 20 to 24 weeks. Place the mother in the LLR position, check BP until stable (may take 10 to 15 minutes), then roll to supine. Check BP right away, then again in 5 minutes. If an increase between the two recordings exceeds 20 mm Hg, the woman is at risk (positive roll-over test).
- Weight is checked every visit. Weight gain pattern should be monitored to determine any abnormalities. This is more important than the amount of weight gain; failure to gain weight is an ominous sign. The prepregnant weight is ideally from 90 to 150 lbs. Normal weight gain patterns contribute to the health of the mother and fetus. The total expected weight gain of 20 to 25, max of 35 lbs. is gained as follows:
- First Trimester: 1 lb. every month, 3 to 4 lbs. in total
- Second Trimester: 0.9 to 1 lb. every week, 10 to 12 lbs. in total
- Third Trimester: 0.5 to 1 lb. every week, 8 to 11 lbs. in total.
- Urine Testing: Benedict’s test (ideally at most 1+), Acetic Acid Test (should be negative)
- Fetal Growth and Development Assessment
- Obstetrical History: A.K.A. OB Scoring; a record of preceding pregnancies and perinatal outcomes. Multiple systems are used:
- 4-Point System (FPAL):
- Full-term: number of full-term births
- Premature: number of premature births
- Abortion: number of abortions
- Living: number of currently living children
- 5-Point System (GFPAL): the addition of Gravida (number of pregnancies) to the 4-Point system.
- 7-Point System (GPTPALM):
- Gravida: number of pregnancies
- Parity/Para: number of deliveries
- Term: number of term children delivered
- Preterm: number of preterm children delivered
- Abortion: number of abortions, not counted as deliveries
- Living: number of currently living children
- Multiple: number of pregnancies with multiple fetuses
- 4-Point System (FPAL):
- Estimates of Pregnancy
- Age of Gestation
- Complete Physical Examination
- Laboratory Testing
Estimates of Pregnancy
- Naegele’s Rule (EDC, EDD): add seven days to the first day of the last menstrual period (LMP), and subtract three months, and one year.
- Ex:
- LMP/Gestational Age/Menstrual Age: calculation of the duration since the last menstrual period. Ovulatory age or fertilization age is calculated from the time of ovulation or fertilization. These are two weeks shorter. LMP dating has a 95% prediction interval of ±4.65 weeks (Lee et al., 2020). Mothers may also be unsure of their last menstrual period.
- McDonald’s Rule: determination of AOG based on fundal height (FH) used in the second and third trimesters. Measure the distance from the top of the symphysis pubis over the curve of the abdomen to the top of the uterine fundus using a tape measure.
- AOG in lunar weeks:
- AOG in lunar months:
- Bartholomew’s Rule of Fours: estimates gestational age based on fundic height. Prior to examination, the mother needs to void.
- FH at Symphysis Pubis: 3 months
- FH between the symphysis pubis and umbilicus: 4 months
- FH at Umbilicus: 5 months
- FH just above umbilicus: 6 months
- FH between the umbilicus and xiphoid process: 7 months
- FH just below the xiphoid process: 8 months, or late 9th month due to lightening.
- FH at Xiphoid Process: early 9th month
- Estimated Fetal Weight (EFW):
- Johnson’s Rule: utilizes fundal height to estimate fetal weight, and varies based on engagement.
- if not engaged
- if engaged
- Johnson’s Rule: utilizes fundal height to estimate fetal weight, and varies based on engagement.
- Estimated Fetal Length (EFL):
- Haase’s Rule: utilizes gestational age to estimate the fetal length in centimeters.
- First five months of the pregnancy:
- Second half of the pregnancy:
- Haase’s Rule: utilizes gestational age to estimate the fetal length in centimeters.
Complete Physical Examination
Internal Examination is done to detect early signs of pregnancy: Chadwick’s, Goodell’s, and Hegar’s sign. The following are the preparations for IE:
- Explanation of the procedure
- Voiding before IE
- Proper positioning: Lithotomy; remember to set stirrups at equal height, avoiding pressure on the popliteal region, and to place legs on stirrups simultaneously.
- Draping
- Instructions for the patient: place the hands across the chest; correct breathing with slow, chest breaths.
WARNING
- Do not perform any activity that increases intra-abdominal pressure.
- Do not distract a woman’s attention from focused breathing/relaxation techniques.
- Avoid any impediment to communication.
Leopold’s Maneuver
Column
Leopold's Maneuver is a systematic abdominal palpation to estimate fetal size, locate fetal back and parts, and determine fetal position and presentation.
- Explain the procedure and its purpose.
- Position: dorsal recumbent with knees slightly flexed to relax the abdominal muscles.
- Draping
- Examining hands should be warm to avoid contractions of the abdominal muscles, which may impede palpation.
- Apply gentle, firm palpations with the palms of the hands.
The steps are divided into four:
- Palpate the fundus; check for breech or cephalic; usually breech— soft, globular, non-ballotable.
- Palpate the sides of the abdomen; check for a smooth, resistant back and irregular, small fetal parts of the fetus. The area of the fetal back is the best site for FHT auscultation.
- Palpate the area just above the symphysis pubis; check for cephalic or breech, usually cephalic; check the position and mobility of the head.
- Palpate the midline downward and just about two inches from the Pourpart’s ligaments; check for position and descent of the head (engagement), including degree of flexion (attitude).
Infobox
Leopold's Maneuver
Step Aliases
Step Name LM1 Fundal Grip LM2 Lateral Grip LM3 Pawlick’s Grip LM4 Pelvic Grip
The Intrapartal Period
Reference
Salustiano, R. (2024). The Intrapartal Period. In Dr. RPS Maternal & Newborn Care: A Comprehensive Review Guide and Source Book for Teaching and Learning (2nd ed., pp. 222-261). C&E Publishing, Inc.
Theories of Labor Onset
The intrapartal period contains a series of physiologic and mechanical processes by which all the products of conception (baby, placenta, and fetal membranes) are expelled from the birth canal. Labor is also called travail, accouchement, parturition, and confinement. The woman in labor is called the parturient. The real cause of labor is unknown, but there are various theories of labor:
- Uterine Myometrial Irritability/Uterine Stretch Theory: considered as the most acceptable theory; when the uterine muscles get stretched with fetal growth and increasing amniotic fluid, it results in irritability and contractions to empty the contents of the uterus.
- Low Progesterone Theory/Progesterone Deprivation Theory: labor is said to start when progesterone (a uterine muscle relaxant) decreases and uterine muscle stimulants increase in late pregnancy.
- Oxytocin Theory: the pressure of the fetal head on the cervix in late pregnancy stimulates the posterior pituitary gland to secrete oxytocin, which causes uterine contractions.
- Estrogenic, Fetal Hormone, and Prostaglandin Theories: all of these have a stimulating effect on the uterine musculature, causing uterine contractility.
- Theory of Aging Placenta: as the placenta matures, more pressure is exerted on the fundal portion, the usual placental site, and the most contractile portion of the uterus. It is believed that the resultant diminished blood supply to the area causes contraction.
Premonitory Signs of Labor
- Lightening: the descent/dipping, dropping of the presenting part to the true pelvis. Engagement is not the same as lightening. The head is said to be “engaged” when the largest diameter of the presenting part passes through the pelvic inlet or the pelvic brim. This occurs earlier in primigravidas, at one to two weeks before labor, and later in multigravidas, at one to two days before labor. There are various signs of lightening:
- Relief of dyspnea
- Relief of abdominal tightness
- Increased frequency of urination, varicosities, and pedal edema because of pressure on the bladder and pelvic girdle
- Shooting pains down the legs because of the pressure on the sciatic nerves
- Increased amount of vaginal discharge
- Braxton Hicks Contractions are another sign, beginning 3 to 4 weeks before labor. They are painless and false labor contractions, appearing intermittently, irregularly, and non-progressively. They do not progress cervical dilatation or effacement, produce abdominal (not lumbosacral) discomfort, and can be relieved by walking and enema. They last anywhere from 30 to 120 seconds, maybe feeling like a wide belt tightening around the front of the abdomen.
- Increased maternal energy/burst of energy because of the hormone epinephrine
- Slight decrease in maternal weight by 2 to 3 lbs, 1 to 2 days before labor. Before labor, there is a drop in the blood level of progesterone, a water-retaining hormone, causing the excretion of retained fluid.
- Show: blood-tinged mucus discharged from the cervix shortly before or during labor.
- Ripening of the Cervix: becomes soft as butter.
- Rupture of the Bag of Waters: an occasional sign. It is an indication for hospitalization.
- Progressive Fetal Descent
- Increased backache and sacroiliac pressure due to fetal pressure.
| Criteria | True Labor | False Labor |
|---|---|---|
| Contractions | Regular, progressive | Irregular, non-progressive |
| Discomfort | Lumbo-sacral radiating to the front; increasing intensity | Abdominal |
| Cervix | Dilated; the most important sign | No dilatation |
| Walking | Intensifies contractions | No effect on contraction |
| Enema | Intensifies contractions | No effect on contraction |
| Show | Present and increasing | Absent |
Physiologic Alterations in Labor
- Dilatation: progressive opening/widening of the cervical os. It is expressed in centimeters, described as “opening”, “widening”, “enlarging”, or “increasing in diameter”. It specifically refers to the cervical external os (a cervical dilatation of 3 cm means the cervical external os is 3-cm open). 10 cm is a fully dilated cervix, the end of the first stage of labor.
- Effacement: thinning and obliteration of the cervical canal. It is expressed in percentage, described as “thinning”, “shortening”, or “narrowing”. A 100% effaced cervix is a fully effaced cervix where the cervical canal has become paper thin or is already absent.
- Physiologic Retraction Ring: the separation of the active, shorter, thicker upper uterine segment an the passive, longer, and thinner lower segment. The Bandl’s Ring is a pathologic retraction ring, formed when the upper uterine segment is as active as the lower segment; seen as an abdominal indentation ring, signifying impending rupture of the uterus if not managed.
Components of the Labor Process (5 Ps)
Power
- Uterine Contractions: the primary power of labor. An involuntary, rhythmical, regular activity of uterine musculature. It occurs intermittently by allowing for a period of uterine relaxation between contractions; uterine and maternal rest and restoration of uteroplacental circulation; sustained fetal oxygenation. This propels the presenting part downward or forward, and aids in progressing dilatation and effacement.
- Contractions increase maternal BP due to increased peripheral arteriole pressure. Measurement of BP should be between contractions to gain accurate results.
- Myometrial contractions constrict blood vessels, decreasing uteroplacental circulation. As such, prolonged uterine contractions can cause fetal hypoxia.
- Contractions can be graphed into three parts, and have relevant durations, intervals, and frequency:
- Increment: increasing or “building up” contraction; the first and longest phase.
- Acme: the apex, height, or peak of the uterine contractions.
- Decrement: the phase of decreasing contraction; “letting up”. The last/end phase.
- Duration: the period from increment to decrement. Measured in seconds.
- Contractions lasting more than 90 seconds can lead to fetal distress, and is called a tetanic contraction.
- Interval: the period from the end to the start of another contraction. It is the uterine resting time, and should be at least 1 minute, not less than 30 to 45 seconds. It is measured in minutes.
- Frequency: the period from the start of one contraction to the start of the next contraction. It is effectively duration plus the interval. Measured in minutes.
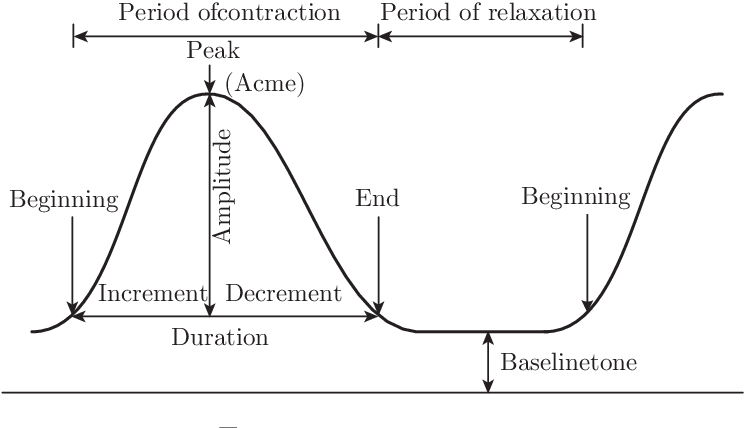
Palpation of Contractions
Place the hand lightly on the fundus with the fingers spread; described as mild, moderate and strong by judging the degree of indentability/depressability of the uterine wall during acme. If indentation is not possible, the contraction is strong; difficulty, moderate; and mild if tense but easily indented.
- Secondary Powers: maternal bearing down/pushing. Only done on full dilation (10 cm), and a fetal station of +1 (able to stimulate the Ferguson reflex, which is triggered by pressure on the pelvic floor).
- Bearing down should not be done prior to full dilation due to the risk of lacerations.
- Teach the mother to take a deep breath as soon as the next contraction begins, and then, with breath held, exert a downward pressure exactly as though she were straining at the stool. She should not hold her breath for longer than six seconds, during pushing. Involuntary pushing, grunting, groaning, exhaling, or breath-holding for less than seconds is supported. She should push four or more pushes per contraction.
Passenger
Refer to The Fetus During Labor.
Passageway INC
Divided between the soft passages: cervix, vagina, and perineum (potentially lacerated) and bony passages: the pelvis. Problems of the bony pelvis that can influence the progress of labor include heredity, a contracted pelvis due to avitaminosis D or rickets in childhood, infection, accidents, and cephalo-pelvic disproportion (CPD), the leading cause of primary cesarean section.
Work Deferred. Watch the Video Lecture on Fetal Skull-Pelvis Relationship
Psyche
A pregnant woman’s general behavior and influences on her also affect labor progress. Some factors that make labor meaningful, positive or negative, even:
- Cultural influences integrating maternal attitudes; how a particular society views childbirth
- Expectations and goals for the labor process, whether realistic, achievable, or otherwise
- Feedback from other people participating in the birthing process.
This also includes the pregnant woman’s psychologic response to uterine contractions; fear and anxiety affect labor progress. A woman who is relaxed, aware of, and participating in the birth process usually has a shorter, less intensive labor.
Placenta INC
Cardinal Movements/Mechanisms of Labor
During labor, the fetal head and body must change positions to accommodate the irregular maternal pelvis. These positional changes are termed the cardinal movements, otherwise called the mechanisms of labor, namely: (mn. D-FIRE-ERE)
- Engagement: the mechanism by which the greatest transverse diameter of the fetal head (biparietal diameter) passes through the pelvic inlet; the head is fixed in the pelvis.
- Descent: the first requisite for the birth of the baby: the progression of the fetal head through the pelvis. This may occur earlier in a nulliparous woman, and usually begins with engagement in a multiparous woman. The degree of descent is measured by station. It spans from -5 to +5, with 0 at the level of the ischial spines. Each interval measures 1 cm above or below the ischial spines. There are four forces of descent:
- Amniotic fluid pressure; thus, some obstetricians elect to rupture the bag of water with an amniotone (amniotomy) to enhance labor progress
- Direct pressure of the contracting fundus/uterus upon the breech
- Effects of contractions on the diaphragm and abdominal muscle contraction
- Fetal body extension and straightening
- Flexion: the mechanism that occurs when the head meets resistance from the cervix, pelvic floor, and pelvic walls, causing the head to flex so that the chin is brought into contact with the chest. This results in the smallest anteroposterior diameter of the fetal head (suboccipitobregmatic diameter: 9.5 cm) to present into the maternal pelvis.
- Internal Rotation: this mechanism involves the turning of the fetal head from left to right, aligning it with the long axis of the maternal pelvis and causing the occiput to move anteriorly toward the symphysis pubis.
- In internal rotation, the fetal skull rotates from transverse to anteroposterior at the pelvic outlet, which is associated with descent.
- After internal rotation, the occiput is just under the symphysis pubis.
- Not accomplished until the head is engaged; occurs mainly during the second stage of labor.
- Extension: the delivery of the head in vertex presentation, or when the head leaves the pelvic outlet.
- There is a gradual emergence of the occiput just under the symphysis pubis, followed by the face and then the chin.
Meconium Aspiration
As soon as the head is out, even before the chest is born, the mouth and then the nose are wiped clear of secretions to prevent meconium aspiration. Routine suctioning of the newborn is no longer performed in the immediate care of the newborn.
- Restitution: after the head is extended, the neck is twisted, so the head needs to externally rotate to realign with the long axis of the fetus.
- External Rotation: as a continuation of restitution, the shoulders align with the anteroposterior diameter, causing the fetal head to continue to rotate. The trunk navigates through the pelvic cavity, with the anterior shoulder descending first.
- Expulsion: final birth of the baby. A gentle but firm downward pressure/traction of the head is done to deliver the anterior shoulder. Then, the head is gently raised to deliver the posterior shoulder, and the entire body follows without much difficulty. The head is the biggest part of the baby; after the head passes out, the rest of the body follows with no difficulty.
- When the entire body of the baby emerges from the birth canal, birth is complete. The time of birth is recorded and entered in the birth certificate.
- Apply Unang Yakap or the Essential Newborn Care (ENC) protocol if part of the institutional practice.
Contact the Healthcare Provider or Go to the Hospital
- When contractions are regular and becoming increasingly frequent: their duration is 30 seconds and they occur every 5 minutes.
- When show is present.
- When the bag of water ruptures. The rupture of the bag of water is always an indication for seeking medical help.
Stages of Labor
Dilatation Stage
The Dilatation Stage begins with the onset of the first true labor contraction up to full cervical dilatation (10 cm). Power comes from uterine contractions. This stage is further subdivided into three phases:
| Latent | Active | Transition | |
|---|---|---|---|
| Dilatation | 1 cm - 4 cm | 4 cm - 8 cm | 8 cm - 10 cm |
| Effacement | Usually complete in primigravidae | Complete effacement | Complete effacement |
| Frequency | >10 min | 3 min - 5 min | 2 min - 3 min |
| Duration | 30 sec | 45 sec - 60 sec | 60 sec - 90 sec |
| Intensity | Mild | Moderate | Strong |
| Behavior | Cooperative | Anxious | Uncooperative |
| Discomforts | - Backache - Abdominal Cramps | - Hyperventilation - Respiratory Alkalosis | - Backache - Pressure on the bladder and rectum - Leg trembling |
| Interventions | - Positioning, Backrub - Companion of Choice | - Drugs for comfort (4 to 6 cm, avoids fetal distress) - Encourage slow breaths or rebreathing with a paper bag or cupped hands. | - Physical comfort with dry linens and cool clothes - Clean up vomitus - Provide a backrub - Coach on breathing technique: pant-blow pattern - Provide psychologic comfort |
| Every pregnancy and birth is unique, so the best intrapartum care for each woman and her baby is individualized, person-centered, respectful, and evidence-based. In the first stage of labor upon admission to the labor unit, greet the patient, admit and orient them to the physical setting and common procedures, and take their history (GPTPALM, EDC/EDD, last meal, allergies, onset of labor, status of bag of waters, intent to breastfeed). Assess their knowledge about labor and preparedness. Take initial vital signs and FHT. |
- Perform Leopold’s Maneuver. Remember to empty the bladder, flex the knees, and warm hands.
- Do perineal preparation; observe the principles of asepsis.
- Render an enema only if ordered. Removal as a routine procedure reduces infection, labor retardation, and postpartum discomfort.
- Obtain specimens for laboratory: urine (sugar, protein, acetone) and blood (Hgb, Hct, WBC, serology, cross-matching).
Monitor for uterine contractions, the bladder, FHT, perineum (Show), rupture of BOW, presenting part, bulging, cord prolapse, bleeding; ability to manage pain.
- BP, PR, and RR every hour in the latent and active phases, and every 30 minutes in the transition phase (if normal).
- Temperature every 4 hours (if normal), and hourly if above 37.5°C or if membranes rupture (leading complication of prolonged rupture of the bag of water is infection).
- FHR: every 30 minutes in the latent phase, every 15 minutes after (if normal).
Prevent supine hypotensive syndrome. Position the patient in a left lateral recumbent position. Employ physical and psychologic comfort and support; comfort measures such as assisting with positional change, keeping clean and dry, and promoting sleep and adequate rest are observed.
- Distraction is one of the methods used to increase relaxation and cope with the discomfort of labor when contractions are mild to moderate. Examples include “happy thoughts”, conversation, light activities (reading, card play, ambulation), and visualization.
- Massages, particularly effleurage, is a light abdominal stroking, which may be used in the first stage to maintain relaxation of the abdominal muscle; effective for mild to moderate pain.
- Back ache is particularly severe in occipitoposterior positions. Pain may be relieved by counter-sacral pressure and a side-lying position.
Always watch for DANGER SIGNALS
- Hypertonic or hypotonic contractions
- Bleeding (placenta previa, abruptio placenta, uterine rupture)
- Passing of meconium-stained amniotic fluid (fetal distress)
- Severe headache, dizziness, and blurring of vision (PIH)
Delivery/Expulsion Stage
The Delivery/Expulsion Stage lasts from full cervical dilatation to the delivery or expulsion of the baby. This stage features the inclusion of secondary powers (maternal pushing, intraabdominal pressure) in the birthing process.
Pushing in the Crowning Stage
Pushing spontaneously occurs with contractions, but panting should be done during interval and at crowning time. Crowning is the hallmark of the second stage. At this period, pushing is not recommended as the fetus undergoes extension, and alteration with pushing can cause perineal lacerations, and meconium aspiration.
- The strength, duration, and frequency of contractions do not vary from the transition phase.
- The perineum bulges; the mother grunts when pushing. There is an increase in show, leg cramps can occur, and the bag of water ruptures. This stage is the best time for rupture. The first nursing action after rupturing is to check the FHT.
Nursing Implementation
- Continue to offer a psychological support and inform the mother of progress. Use (mn. PRAISE) Praise, Reassurance, Encouragement, Informing the mother of progress, Support System (COC), and Therapeutic Touch.
- Assist/Coach through labor, about when to push or to pant.
- Monitor FHT during intervals (period of rest). If there is a continuous fetal heart electronic monitor, check the FHT during and after a contraction. Be alert for late decelerations.
- Transfer the mother to the delivery room. For primigravidas, with slower progress of labor, they are transferred at 10 cm of dilatation with a certain degree of bulging with contractions. For multigravidas, they are transferred at 8 to 9 cm.
- Positioning: lithotomy with padded, equal stirrups, with no pressure on the popliteal region. The legs are placed on the stirrups simultaneously. Alternatively, Fowler’s, side-lying, or squatting can be used if desired, indicated, or supported by the unit policy.
- Perineal Preparation: cleaning of the perineum to prepare for delivery. A front-to-back motion is used.
Placental Stage
The Placental Stage is the period from the delivery of the baby to the delivery of the placenta. The powers involved in the delivery of placental delivery is from strong uterine contractions, and maybe maternal pushing once the placenta has fully detached. There are four primary signs of placental separation:
- Calkin’s sign: the first sign; when the uterus changes shape (from discoid to globular) and consistency (becomes firm).
- Uterine mobility: the uterus rises up into the abdomen. Immediately after placental detachment, the fundus is midway between the symphysis pubis and umbilicus, then rises to the level of the umbilicus.
- Sudden gushing of blood from the open blood vessels once connected to the placenta. It is important to distinguish between the normal sudden gushing of blood, and the abnormal “increasing bleeding”.
- Slight lengthening of the cord: the most definitive sign that the placenta has detached.
The placental delivery can be typed according to which side of the placenta appears first:
- Schultze Mechanism: more common; present in 80% of cases. The shiny, “clean”, bluish side is first delivered. Less external bleeding occurs because blood is usually concealed behind the placenta. The separation for the placenta in this type starts with the middle, then to the edges, which gives it an “inverted umbrella” appearance.
- Matthew Duncan Mechanism: present in the remaining 20% of cases. The rough, “dirty”, reddish side is first delivered. More external bleeding occurs, giving the delivery a “bloody” appearance. The separation for the placenta in this type starts with the side, giving it an “umbrella” appearance.
Postpartal Hemorrhage
The normal amount of blood lost in the entire process of delivery is 250 to 300 mL. Blood loss of more than 500 mL is considered postpartal hemorrhage, the leading cause of maternal mortality.
Nursing Implementation
Observe the principles of the placental delivery stage:
- Watchful Waiting (watch and wait for signs of placental separation)
- Not Increasing Fundal Pressure with a pull at the cord, especially if the uterus is relaxed, as these actions could cause uterine inversion, a leading cause of hemorrhage in the third stage of labor.
- Gradual Delivery of the Placenta
- Inspect the placenta for completeness. The major components of a placenta are cotyledons (15 to 20), cord vessels (two arteries and one vein), and complete membranes. This ensures the reduction of potential placental fragment retention, causing hemorrhaging.
Assess the uterus for contraction or firmness. The terms “soft,” “boggy,” and “non-palpable” mean uterine atony. The initial activity of the nurse is to massage the fundus until it is firm. An ice cap may be applied to further contract the uterus, but never a hot water bag. This promotes vasodilation, increasing bleeding.
Oxytocin is ordered by the physician and administered by the nurse after placental delivery. Commonly used drugs include methergine (Methylergonovine maleate) and ergotrate (Ergonovine maleate/Ergometrine). These increase uterine motor activity by direct stimulation of the uterine musculature. Contraction prevents postpartum bleeding from uterine atony and subinvolution. Evaluate for a firm fundus to determine effectivity. This may cause nausea, vomiting, dizziness, headache, hypertension, tinnitus, and hypersensitivity.
After the birthing process, assess vital signs, presence of lacerations, completeness of the placenta, and bleeding. Lower legs slowly. If allowed by the institution, allow mother time with the infant to promote attachment or bonding; breastfeed right on the delivery table.
Recovery
The Recovery Stage is the period of recovery, stabilization, or homeostasis; usually 1 to 2 hours or at most up to 4 hours. Power still remains from uterine contractions that prevent bleeding from the placental site.
- Vital signs every 15 minutes. Blood loss averages 250 mL during delivery. A normal upper limit is 500 mL. More than this amount is defined as postpartum bleeding.
- Blood pressure changes (lower in both systolic and diastolic, increased pulse pressure, slight to moderate tachycardia) occur from blood loss, lifting of the uterus, and redistribution of blood to the venous beds.
- Palpate the fundus every 15 minutes. Check fundal height and position in relation to the umbilicus, and its consistency. In a normal delivery during the recovery stage, the fundus is firm, midline, and at the level of the umbilicus.
- Ask the mother to void prior to any palpation. This promotes maternal comfort and improves finding accuracy from palpation.
- Displacement of the uterus to the side is often due to a distended bladder. Palpate the lower abdomen for a distended bladder, and if it is, stimulate voiding. Displacement can contribute to uterine atony.
- Assess Lochia. Lochia is bright-red during the fourth stage, and can saturate one to two pads in one hour. A reddish color may be maintained for two weeks, but longer periods indicates either retention of small portions of the placenta or imperfect involution of the placental site, or both.
| Parameter | Rubra | Seroa | Alba |
|---|---|---|---|
| Color | Red | Brownish | White |
| Amount | Moderate | Scanty | Slight |
| Time Present | 1 to 3 days | 4 to 10 days (average and at least 7 days) | 10 to 14 days (at most 21 days) |
- Assess the perineum. Note its general appearance, redness, swelling, bruising, and vaginal and suture line bleeding.
- Administer oxytocin medication as ordered. Check blood pressure before and at intervals after; monitor fundal contraction and lochia after administration.
- Check the episiotomy wound or lacerated wound for bleeding, hematoma, or edema. An ice bag applied to the perineum immediately after delivery (and in the first 24 hours) can reduce edema and swelling.
- Promote sleep and comfort. Keep the mother warm, as chills are common in the fourth stage. This may be due to maternal excitement, a sudden drop in maternal hormones (progesterone is thermogenic), the release of intra-abdominal pressure, and fetal blood in circulation.
- Perform a partial bath and peri-care (front to back), and changing wet linens.
- Assess for afterpains; pains that occur upon uterine contraction. Reassure that these are secondary to uterine contractions. An icecap may be placed on the abdomen overlying the fundus for relief, or analgesics may be given as ordered.
- Provide nourishment. The mother may be thirsty and hungry.
Always Provide Respectful Care
Remember that the care of maternity clients should always be respectful. Respectful intrapartum care maintains women’s dignity, privacy, and confidentiality, ensuring freedom from harm and mistreatment, and enabling informed choice during labor and childbirth. This WHO model of intrapartum care provides a basis for empowering all women to access and demand the type of care that they want and need (WHO, 2020c).
The Fetus During Labor
Reference
Salustiano, R. (2024). The Fetus During Labor. In Dr. RPS Maternal & Newborn Care: A Comprehensive Review Guide and Source Book for Teaching and Learning (2nd ed., pp. 262-270). C&E Publishing, Inc.
Column
clean
Fetal Head
The fetal head has seven bones. Two frontal, two parietal, two temporal, and one occipital. Along the adjacent edges of these bones are sutures, and the meeting points of multiple skull bones are fontanels.
- Sagittal Suture: longitudinal, midline
- Frontal Suture: anterior suture between two frontal bones.
- Coronal Suture: anterior suture between frontal and parietal bones.
- Lambdoidal Suture: posterior suture between parietal and occipital bones.
INFOBOX
Fetal Skull
- Anterior Fontanel: formed by two frontal bones and two parietal bones. It is diamond-shaped, measures 2.5 cm × 2.5 cm, and ossifies in 12 to 18 months.
- Posterior Fontanel (Lambda): formed by the union of two parietal bones and one occipital bone. It is triangular and ossifies in 6 to 8 weeks or 2 to 3 months.
| Fetal Skull Diameters | ||
|---|---|---|
| Anteroposterior Diameters | Width | Description |
| Occipitomental | 12.5-13.5 cm | Widest; from the occiput to the chin. |
| Occipitofrontal | 12 cm | From the occiput to midfrontal bone |
| Suboccipitobregmatic | 9.5 cm | Narrowest; from below the occiput to the anterior fontanel. |
| Transverse Diameters | ||
| Biparietal | 9.5 cm | Widest; distance across the two parietal bones. |
| Bitemporal | 8 cm | Distance across the two temporal bones. |
| Bimastoid | 7 cm | Distance between the two mastoid processes. |
Fetal Lie
The relationship of the long axis of the fetus to the long axis of the mother’s uterus/spine.
- Longitudinal: the fetal and maternal axes are parallel. This can be further classified as cephalic or breech presentation depending on which part enters the pelvis first.
- Transverse Lie: the long axis of the fetus is perpendicular to the mother’s spine; shoulders present.
Fetal Attitude
The relationship of the fetal parts to the trunk or to one another.
- Flexion: the desired attitude.
- Extension
Fetal Presentation
The lowermost part in the pelvic inlet; the part felt upon internal examination.
- Cephalic: the head is the presenting part.
- Vertex: head acutely flexed (suboccipitobragmatic, 9.5 cm)
- Sinciput: head moderately flexed
- Brow: head moderately extended
- Face: head acutely extended (mento-vertical, 13.5 cm)`
- Breech: the buttocks are the presenting part. FHT is felt at the upper quadrants or above the level of the umbilicus, and with the findings of Leopold’s maneuvers 1 (hard, round, ballottable mass) and 3 (soft, globular, non-ballottable mass).
- Complete (Full): feet and legs are flexed on the thighs; buttocks and feet presenting; fetus squatting; the type favoring most the second stage of labor as the feet could be used as traction.
- Incomplete (Frank): thighs flexed against the abdomen; legs extending up to the shoulders as they lie on the anterior chest; buttocks present; the type favoring most the first stage of labor as the large buttocks are a good dilating wedge.
- Footling (single or double): one foot or two present; the type is easily complicated by cord prolapse.
Meconium Staining
If the fetus is breeched, the passage of meconium staining is not a sign of fetal distress.
- Shoulders: usually referred to as a transverse lie; the fetal long axis lies perpendicular to the maternal spine, and the fetus appears to lie crosswise in the uterus.
Fetal Position
Position refers to the relationship of the denominator or landmark of the presenting part to the front imaginary quadrants of the mother’s pelvis. Assessment of the position can be done through Leopold’s maneuvers, vaginal examination, and rectal examination (obsolete).
- Chosen Landmarks/Denominators:
- Occiput (O) for vertex presentation
- Mentum (M) for face presentation
- Sacrum (S) for breech presentation
- Acromiodorso (AD) for shoulder presentation
- Four Imaginary Quadrants:
- Left anterior
- Right anterior
- Left posterior
- Right posterior
| Occiput | Mentum | Sacrum | Acromiosdorso | |
|---|---|---|---|---|
| Left Anterior | LOA | LMA | LSA | LAPA |
| Right Anterior | ROA | RMA | RSA | RAPA |
| Left Posterior | LOP | LMP | LSP | LAPP |
| Right Posterior | ROP | RMP | RSP | RAPP |
- Left occipitoanterior (LOA) features the occiput pointing towards the mother’s left abdominal wall, face is down towards the maternal right buttocks; most common and favorable position.
- Occiputposterior (OP), either left (LOP) or right (ROP), is a factor in prolonged labor, with the mother experiencing much discomfort (backache) during labor. Comfort measures: side-lying, backrub, counter-sacral pressure during contractions.
Column
Note
Fetal Station
Station refers to the relationship of the presenting part to the ischial spines, the single most important landmark of the pelvis. It measures how far the presenting part has descended into the pelvis— the degree of descent. Each station is one centimeter and determined through internal examination.
- Floating (High; Ballottable): unengaged presenting part
- Station 0: the presenting part is at the level of the ischial spines.
- Minus Station (Negative): if the presenting part is above the level of the ischial spines, station is expressed as a negative number (e.g., -1 (1 cm above), -2 (2 cm above)).
- Plus Station (Positive): if the presenting part is below the ischial spines (outlet), station is expressed as a positive number (e.g., +1 (1 cm below), +2 (2 cm below)).
Infobox
Stations
Score Meaning -5 to 0 The “presenting” or most palpable (able to feel) part of the baby is above the woman’s ischial spines. 0 The baby’s head is known to be “engaged,” or aligned with the ischial spines. 0 to +5 Positive numbers are used when a baby has descended beyond the ischial spines. During birth, a baby is at the +4 to +5 station.